By Evette Ramirez, DPT, DOR, Legend Oaks of Waxahachie, TX
All information taken from the Vestibular course given by Ann H. Newstead, PT, DPT, PhD, GCS, NCS, CEEAA (https://www.ahnewphysicaltherapy.com/)
 As we age, there is a greater incidence of falls. Many factors play a role in these falls; some external and some internal. Some risk factors include medications and resulting side effects, cognitive impairments, lower extremity disability including loss of sensation and/or foot deformities, balance abnormalities, dizziness, orthostatic hypotension as well as increased dependence on visual cues for ability to achieve and maintain balance.
As we age, there is a greater incidence of falls. Many factors play a role in these falls; some external and some internal. Some risk factors include medications and resulting side effects, cognitive impairments, lower extremity disability including loss of sensation and/or foot deformities, balance abnormalities, dizziness, orthostatic hypotension as well as increased dependence on visual cues for ability to achieve and maintain balance.
Vestibular function is an area that we as clinicians can address to help reduce potential falls. As 30% of older adults develop vestibular dysfunction, knowledge of when and how to treat as well as when to refer to a specialist is a needed skill. As we age, vestibular changes begin at age 40 with reduced number of hair cell in the inner ear as well as a decreased number of nerve fibers, which lead to decreased to increased difficulty with competing visual and somatosensory input.
Definitions to know:
Vertigo: an illusionary sensation of motion of either the self or the surroundings in absence of true motion.
Oscillopsia: a visual illusion of oscillating movements of stationary objects. This can arise with lesions of the peripheral or central vestibular systems.
Receptor: a patch of hair cells projecting into a gelatinous membrane
Otoconia: calcium carbonate crystals that rest on top of the macula and are floating on tome of the gelatinous membrane. (Gravity and shearing forces occur with acceleration and deceleration and deflection of the hairs.
Semicircular Canals (SSC): ring shaped, fluid filled canals set at 90 degree angles to each other on each side of the head as functional pairs. These work as the push / pull mechanism. Ex. Increased firing of RSSC when turning head to the right will decrease on left.
Vestibular Nuclei: There are four vestibular nuclei in the CNS. These are located in the floor of the 4th ventricle between the medulla and the pons. Visual and somatosensory inputs are integrated here with information entering bilaterally. Information is sent to the brain, cerebellum and to the spinal cord via CN VIII.
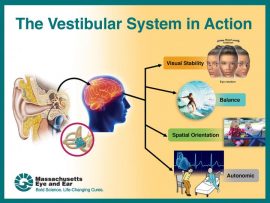
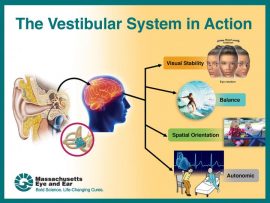
The vestibular system has three main functions: 1) Gaze stabilization which refers to ocular stability. This keeps images stable by moving eyes in response to head movements. 2) Postural control which detects position and movement of head in space; along with sensory and proprioceptive systems. 3) Perception of motion which helps to distinguish eye movements from head movements (internal) and head movements from exocentric (environmental) movements. The vestibular nuclei, cerebellum and reticular formation all receive input form visual and somatosensory systems. The output form these areas influence oculomotor control and spinal motor control. The central pathways for these systems are separate, therefore, both systems are examined and treated separately.
A vestibular exam will typically consist of:
• Acquiring a history
• CN testing
• Eye head coordination
• Positional testing
• Postural control
• Functional testing
• Locomotion
Other assessments include: Visual vertigo analog scale (VVAS)
Dizziness Handicap inventory/index (DHI)
Activity-specific Balance Confidence (ABC) Scale
Clinical decision-making model and differential diagnosis includes:
• Acute symptoms – Possible BPPV, labyrithinitis, stroke , fall and concussion
• Episodic – possible Meneire’s, postural hypotension
• Chronic – Possible Mal debarquement, hair cell loss, aging, long term CNS injury
Exam:
By taking our clients through various positional changes and movements of the head, we can elicit symptoms and this will help to determine where the lesion/dysfunction is originating and lead us to the best protocols to reduce symptoms. Following the steps below, one can observe ocular movements and fluidity of movements, lag in response to positional changes or presence of nystagmus (ticking of eye movements horizontally or vertically). Always take note of direction of the “beat”/tick as well as how long it lasts. Always assess the client’s perception of severity of vertigo on 0-5 scale with 5 being severe.
Visual field deficits: Normal: superior 60 deg; inferior 75 deg; tamporal 100 deg; nasal 60 deg.
Eye / head coordination: Eye range of motion – rectangular; eye coordinated, conjugate motion with head steady.
Smooth pursuit – smooth eye movement at less than 60 degrees per second; eyes tracking moving object
Saccadic eye movements – rapid eye movements between two targets
Vestibular Ocular Reflex (VOR) – gaze stability during rapid head movement
In-phase – eyes fixed on object; heading moving
Cervical Ocular reflex (COR) – rotation of body under head – keeping head stationary
Gaze Stabilization – Optokinetic system
• Combination of saccadic and smooth pursuit system
• Stimulated by repeated movements across a subject’s visual field (an object moving across the stationary visual field or by a person passing by a stationary visual field)
Nystagmus – non-voluntary rhythmic oscillation of eyes; fast and slow components beating in opposite directions; named by the fast component.
• Pathological nystagmus – appear with or without external stimulation in patients with vestibular disorders
• Spontaneous – present with head erect and gaze centered
• Positional – induced with changes in head position
• Gaze evoked – induced by change in eye position
Peripheral Vestibular lesion:
• Jerk nystagmus (named for the fast component: away from the lesion: either up or down beating) Side of lesion is opposite the quick motion (jerk)
• Pendular nystagmus (right or left beating; or up or down beating)
• Rotary nystagmus (named for direction of spin e.g. Upward and rotary)
• Result of asymmetry of right and left vestibular systems.
Head thrust test (HTT) or head impulse test (HIT) – clear neck AROM and carotid artery first
• Fixation on near target then far target ( 6 ft away)
o Slow head movements
o Fast head movements
• Watch for saccades – re-fixate on target (nose)
o Peripheral or central vestibular lesion – unable to maintain gaze
o Bilateral peripheral vestibular lesion – re-fixation to both sides
Head Shaking nystagmus test
• Eyes closed; head tilted downward to 30 deg (places horizontal canals // to ground)
• Turn head passively side to side 20x (2Hz)
• Check for nystagmus using frenzel lenses
o Unilateral peripheral lesion – asymmetrical nystagmus – slow phase toward involved (hypo-functioning) side
o Normal – no nystagmus
o Central lesion – vertical nystagmus
Clinical dynamic visual acuity test (DVAT-N)
• Measures functional VOR or ability for person to stabilize gaze during head movement
• Read visual acuity chart on wall 4 m away
o Lowest line read seated
o Lowest line read while head is passively oscillated in horizontal direction at 2Hz
*Vestibular hypofunction of >3 line change in visual acuity
Monofilament testing plantar sensation
Sensory levels 1= 1g Normal sensation
2= 10 g Protective sensation
3= 75g Loss of protective sensation
4= No perception
Motion Sensitivity quotient (MSQ) – Measures individual response to positional changes. (I.e. quickly supine to side lying R and L; supine to sit and return; wait for response
• Establish baseline of symptoms of vertigo/dizziness, nystagmus at rest
• Monitor symptoms of vertigo/nystagmus
Dix-Hallpike Maneuver
• Quick movement from sitting to sidelying with head rotated 30 deg away from downside ear
• Caution: check for neck AROM and vertebral artery prior to any quick motions of neck on older people
• Watch for nystagmus and direction
• Record duration and intensity of nystagmus and vertigo 0 (none) – 5 (severe)
o Nystagmus directional perponderance:
Horizontal canal – nystagmus will occur with fast component toward the floor (Horizontal geotropic meaning, toward the earth) or Ageotropic – away from the earth
Anterior canal – torsional and DB (down beat)
Posterior canal – torsional and UB (upbeat)
The most common peripheral lesion is BPPV of the posterior canal. With testing, one will typically see and upbeating, torsional nystagmus. (There may be a 30 second delay in nystagmus). Short term is <2 minutes if BPPV. This will usually improve in one treatment. Allow rest and re-test for symptoms.
Evaluation and interpretation of findings
With evaluation, Peripheral lesions/dysfunctions will present with BPPV, nystagmus, short duration vertigo, possible hearing loss and/or tinnitus. While Central dysfunctional will present with head trauma, concussion, stroke, MS. Symptoms will include nystagmus vertically, long lasting, lateropulsion and head tilt.
Mechanical Dysfunctions to look for
• Benign Proxysmal Positional Vertigo (BPPV), with typically be a result of cupulolithiasis or canalithiasis. Symptoms will typically include vertigo with changes in head position, nausea with/without vomiting, disequilibrium
• Right Posterior Cupulolithiasis will typically present with a persistent upbeat nystagmus and right torsion. Canalithiasis will typically present with transient upbeat and right torsion.
• Left anterior Cupulolithiasis will typically present with persistent downbeat and right torsion. Canalithiasis will typically present with transient downbeat and right torsion.
• Horizontal cupulolithiasis will typically present with persistent upbeat nystagmus, while canalithiasis will typically present with downbeat nystagmus
Identification of Semicircular Canal if peripheral lesion:
Canal Involvement Primary nystagmus: right Hallpike-Dix Reversal nystagmus: Right Hallpike-Dix Nystagmus: return to sitting
Right posterior Upbeat and right-ward torsion downbeat and left-ward torsion Downbeat
Right Anterior Downbeat and right torsion Upbeat and left torsion upbeat
Horizontal Horizontal opposite horizontal direction opposite horizontal direction
Left Anterior Downbeat and left-ward tornsion Upbeat and right-ward torsion upbeat
Treatment
In most instances, the techniques presented below will significantly decrease or stop symptoms within 1-2 treatments. Once, vertigo symptoms are addressed, balance, advanced gait and strengthening can be addressed as well as accommodation techniques which will become more complicated/advanced as the client accommodates. These will involve increasing eye, head and body movement as the client improves.
Canalith Repositioning Technique: CRT-Posterior SSC (Canalithesis BPPV) Treating Left side.
• Turn head left 30 deg from midline
• Maintaining 30 deg head turn, move to supine position
• While in supine, turn head to opposite side (right), 30 deg from midline
• Have client roll to onto right side while still maintaining 30 deg head turn to the right
• Transition back to upright position while maintaining 30 deg head rotation
Cupulolithesis (for posterior SSC) Treating Right side
• With client in sitting position, rotate head 30 deg right
• Move to side lying right, maintaining head rotation
• Keeping head at 30 deg rotation from midline, have client sit up and move to side lying Left
• Then move back to sitting. Head will be in original 30 deg to Right.
*once head rotation 30 deg from midline is achieved initially in sitting, this head position is maintained throughout the maneuver.
Cupulolighesis BPPV (for anterior SSC) Treating right side
• Have client in sitting position, turn head 30 deg to left
• Transition to side lying right (with head maintained in 30 deg rotation – head rotation will be up toward ceiling)
• Then move to left side lying while maintaining rotation 30 deg to left – head rotation will be toward the floor)
• Then have client move back to upright sitting, maintaining head rotation to left 30 deg.
Horizontal Canals – Roll Test
• With pt in supine, to test right side, have client rotate head to the right
• To test left side, have client rotate head to the left
*Alternative position can be performed with client’s head on a pillow or wedge
Canalith repositioning technique: CRT – Horizontal SSC
• Start with client in side lying with “bad” ear down
• Roll to supine
• Then move to opposite side lying position with “bad” ear up
• Then move to quadruped position with head // to the floor
Habituation Techniques:
• General habituation technique for posterior SSC BPPV. In sitting position, rotate head 30 deg Left, move to side lying left, then back to sitting, repeat on opposite side. Remain in position 30 sec or until vertigo stops. Perform 10-20 x TID.
• Gaze stability – looking at a fixed object and turning the head slowly from side to side.
o Turning body under the head with head fixed
o Body/head fixed looking at a central object, moving eyes only look to objects above, below, laterally and diagonal to central object/point
o Balance activities – stepping over objects, around objects.
o Gait activities with head movement
The activities outlined above are just a starting point. Be creative and always create an individualized program for each client based on symptoms, persistence of symptoms and each client’s specific deficits, their specific goals and activities and hobbies each client wants to return to.
 One of our initiatives for 2021 is to increase our SLP programming, thus providing a more cohesive and multi-disciplinary approach to care. Hiring SLPs can be challenging depending on the market. One way to increase the number of candidates for SLP positions is to consider hiring a newly graduated SLP, also referred to as a CFY.
One of our initiatives for 2021 is to increase our SLP programming, thus providing a more cohesive and multi-disciplinary approach to care. Hiring SLPs can be challenging depending on the market. One way to increase the number of candidates for SLP positions is to consider hiring a newly graduated SLP, also referred to as a CFY.

 Caitlin Colteryahn is our lead occupational therapist here at The Healthcare Resort of Leawood and has been with us for four years. Caitlin graduated from Rockhurst University in 2014. She has been married for 10 years and has two boys. She loves spending time outdoors and traveling, especially with friends and family.
Caitlin Colteryahn is our lead occupational therapist here at The Healthcare Resort of Leawood and has been with us for four years. Caitlin graduated from Rockhurst University in 2014. She has been married for 10 years and has two boys. She loves spending time outdoors and traveling, especially with friends and family.

 All in the Family
All in the Family
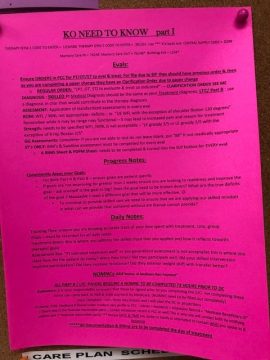 Kristin Ryther, the therapy program manager at Keller, has been a breath of fresh air in a very trying year at a facility that has been hit hard by COVID on multiple occasions. We asked her to share a bit of her best practices and were blown away by what is developing there.
Kristin Ryther, the therapy program manager at Keller, has been a breath of fresh air in a very trying year at a facility that has been hit hard by COVID on multiple occasions. We asked her to share a bit of her best practices and were blown away by what is developing there. gratitude. Kristin has become a champion of championing others. She works to identify strengths in each of her team members and then assigns responsibilities appropriately. Each member has a strength; slow down and find it! It may be that they have special attention to individual treatments; they may be strong at scheduling, growing programs, or even leading the infection control of the gym. List them out and recognize them.
gratitude. Kristin has become a champion of championing others. She works to identify strengths in each of her team members and then assigns responsibilities appropriately. Each member has a strength; slow down and find it! It may be that they have special attention to individual treatments; they may be strong at scheduling, growing programs, or even leading the infection control of the gym. List them out and recognize them.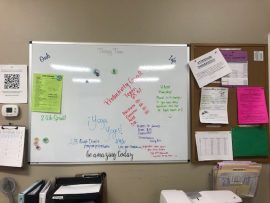 Set clear goals and expectations. Kristin sets goals for “2 week sprints.” Some programs are short projects. She assigns a leader and assists with facilitation but allows for teamwork so they meet their goals. She posts the sprints on the communication board, writes about it, takes pictures and then celebrates it. Short-term goals like this make it manageable, and then the challenge is less likely to be pushed off down the road.
Set clear goals and expectations. Kristin sets goals for “2 week sprints.” Some programs are short projects. She assigns a leader and assists with facilitation but allows for teamwork so they meet their goals. She posts the sprints on the communication board, writes about it, takes pictures and then celebrates it. Short-term goals like this make it manageable, and then the challenge is less likely to be pushed off down the road.

 As we age, there is a greater incidence of falls. Many factors play a role in these falls; some external and some internal. Some risk factors include medications and resulting side effects, cognitive impairments, lower extremity disability including loss of sensation and/or foot deformities, balance abnormalities, dizziness, orthostatic hypotension as well as increased dependence on visual cues for ability to achieve and maintain balance.
As we age, there is a greater incidence of falls. Many factors play a role in these falls; some external and some internal. Some risk factors include medications and resulting side effects, cognitive impairments, lower extremity disability including loss of sensation and/or foot deformities, balance abnormalities, dizziness, orthostatic hypotension as well as increased dependence on visual cues for ability to achieve and maintain balance.
 By Shelby Donahoo, Therapy Resource, Tucson, AZ
By Shelby Donahoo, Therapy Resource, Tucson, AZ