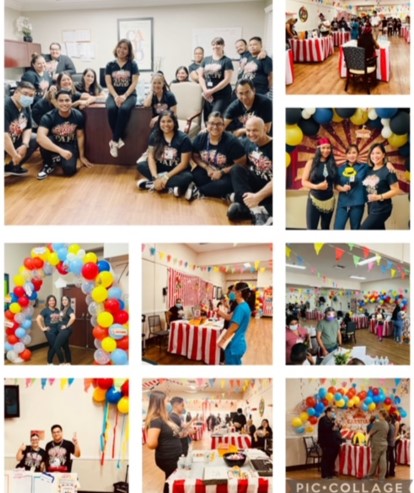
Congratulations Patty Fantauzzo, CTO/COTA/L, TPM, Julia Temple, Englewood, CO
Gaithersburg, MD: The National Board for Certification in Occupational Therapy, Inc. (NBCOT®) announces Patricia “Patty” Fantauzzo, COTA/L, a certified occupational therapy assistant from Castle Rock, CO, has won the 2022 NBCOT Impact Award. This award recognizes certified occupational therapy (OT) practitioners who demonstrate exceptional professional commitment through their dedication, hard work, and outstanding OT skills to improve their clients’ overall life satisfaction.
Patty received the NBCOT Impact Award because of her dedication to providing services for people with Alzheimer’s disease and other dementias. Patty’s colleague Malissa Sanchez, COTA/L, nominated her for the award. At Julia Temple Healthcare, Patty created a therapy program that uses the Abilities Care Approach to ensure long-term care residents who have Alzheimer’s and dementia progress through the disease process with dignity and comfort while maintaining their highest practicable level of cognitive and physical function. Prior to Patty’s involvement, long-term care residents with cognitive impairments at Julia Temple were less likely to receive skilled therapy services. Patty’s approach to providing care is to focus on the residents’ remaining abilities instead of their deficits and to consider what the resident can do or may do based on their preferences. Patty’s team of therapists embraced this philosophy and as a result, they completely transformed the therapy department and the facility as a whole. Through this approach, therapists and physicians also have a better understanding of each resident’s individual abilities and needs, which has enabled them to interact with residents in a more meaningful way. Several program outcomes can be partly traced back to Patty’s work, including a reduction in resident altercations, increased resident independence with certain tasks, and fewer prescriptions for psychotropic medications.
Patty earned her national OT certification in 1995. She is the Therapy Program Manager and Chief Therapy Officer (our highest designation for a Therapy Leader) at Julia Temple Healthcare in Colorado. Patty has shared her knowledge on dementia programming at Colorado Occupational Therapy Association’s annual conference and to dementia support groups and practitioners at Julia Temple. She also assisted two sister facilities in introducing dementia programming to their long-term care services. Patty has received several awards for her work, including the Agatha Jackson COTA Award of Excellence from the Colorado Occupational Therapy Association and the COTA of the Year award from the Arizona Occupational Therapy Association.
For more information about the NBCOT Impact Award, visit www.nbcot.org/awards.