By Tara Meyerpeter, OT, DOR, Keystone Ridge Nursing & Rehabilitation, Omaha, NE
America’s aging population continues to increase in numbers as well as cultural diversity. Baby boomers of all races and nationalities are entering our senior living communities. It is important to embrace cultural diversity and accept the different customs that contribute to the make-up. As the make-up of seniors changes, front-line staff are provided the opportunity to embrace new cultures and celebrate multicultural diversity.
Here’s how to get involved:
- Create an occupational profile to obtain pertinent information regarding ethnicity and cultural background following development of rapport and trust.
- Identify ways to incorporate preferences into treatment sessions (such as recognition of prayer practices, cultural preference/practices, and routines).
- Provide your staff with education to recognize and accommodate the unique needs that accompany different cultures.
- Provide activities and programs that offer seniors the opportunity to experience a variety of cultures such as a multi-cultural showcase.
- Provide interpreters for those who need it, especially in medical situations.
- Enable the use of interpersonal skills to demonstrate intentional respect for resident’s cultures.
- Offer residents with opportunities to express cultural heritage and to learn about cultural identities of others.
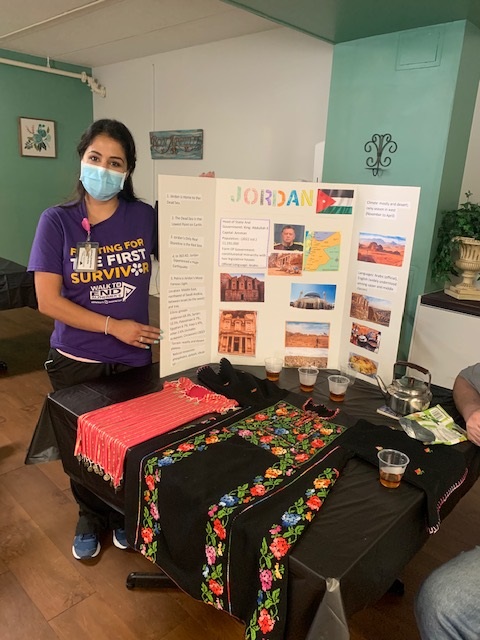
Keystone Ridge celebrates diversity in a multitude of ways. Recently, our OT Woroud (Rosie) Hudson assisted in creating a multicultural diversity group with our residents. Each week for four weeks in the month of August, residents worked on their project to display at our Multicultural Showcase. The residents met every Tuesday for approximately 30 to 45 minutes in preparation for the final presentation. The residents were provided with the level of cognitive assistance needed to fully engage and become immersed in research. Research included reading and locating pertinent information in printed article form and on the internet, locating images to add to posters, and cutting/pasting and organizing printed information on a tri-fold poster to represent countries. Most residents chose countries from which they had ancestry, while others chose countries related to personal interests. Each session, residents reported the history of their country, geography, traditional food and attire, art/music, and shared past experiences. They determined what artifact would be showcased to represent their country, whether it be food, attire, music, or a video displaying their country.
These activities allowed residents to take pride in their accomplishments and promoted an overall sense of both independence and interdependence, which enhanced their quality of life which enhanced QOL. The residents were excited and looked forward to attending the next session/workshop to continue to work on the final project. Residents were motivated to get out of bed and attend workshops during program, which was a motivating factor to increase out-of-bed and out-of-room activity to decrease the risk of excess disability and sensory deprivation. The most powerful benefit accomplished from this program would be the reminiscing-building opportunities developed during the sessions and at final showcase. Residents were able to tap into long-term memories of past experiences related to culture and past traditions and enjoyed sharing past experiences with others.
Countries exhibited included: Italy, Mexico, Poland, Germany, Jordan, and Lebanon.