This new special award, in essence, emulates the spirit and incredible human being that Natalie was.
Natalie was a PT at Legends Euless when it was transitioned by Ensign in the 2016 Legends acquisition. At the time of transition, the DOR decided to leave and remain with the outgoing company. Natalie stepped up to become the DOR. She had not been a manager before, but she worked diligently to learn what she needed to do to lead her new team with a new company and new systems. Natalie truly evolved as a leader, showing ownership for her department, love for her team and compassion for her residents. In fact, Natalie’s facility was leading in best therapy metrics ever and leading us in Keystone when she found out right before last year’s DOR conference in California that she had breast cancer. While this would have stopped many people in their tracks, Natalie persevered. She took the initiative to work from home on days when the treatment kept her down, never giving up hope and never letting her family or her team down. She completed her chemo treatments the first week of January, 2019 and we were all relieved and excited for her! Unfortunately, what we didn’t know was that the chemo had taken its toll. A rare reaction to the treatment had done serious damage to Natalie’s heart. On March 5, 2019, Natalie reported to work in spite of feeling horrible. She used a facility walker to attend the morning meeting before her team sent her home. She went to the ER where the damage to her heart was eventually discovered but irreparable. We lost Natalie in the early morning hours of March 7, 2019. While Natalie was enduring treatment, her ADOR Kim Graybeal readily stepped up and filled in the gaps. She attended meetings, triple checks, assisted with staffing/scheduling and held the team together in moments of fear, chaos, and uncertainty.
When Natalie passed, we knew there was really only one person who could help the Euless team make such a difficult transition. Kim Graybeal has eased the burden with grace and dignity. She carries Natalie’s memory in high esteem and continues to hold their team together in ways that few others could. In spite of the huge void left by our beloved Natalie, we award Kim with the first annual Natalie Blascienski Award to recognize how she has stepped up in the face of adversity, shown leadership in times of turmoil, and displayed unconditional love to her team, her facility, and to Natalie and her family—many traits that Natalie possessed. Please join me in congratulating Kim Graybeal, DOR of Legend Euless, as we honor her with this prestigious award.




 Deciding the Principle Medical Diagnosis, By Lori O’Hara, MA, CCC-SLP
Deciding the Principle Medical Diagnosis, By Lori O’Hara, MA, CCC-SLP
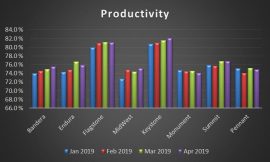
 As we move closer to the October 1st changes with PDPM, many therapy programs have made concerted efforts to implement Group and Concurrent modes of treatment and have noted how their patients are enjoying them. Since January of 2019 we can see a significant shift to adding multi-patient treatment programming across several affiliated companies. The chart below shows a steady increase month-over-month for 2019.
As we move closer to the October 1st changes with PDPM, many therapy programs have made concerted efforts to implement Group and Concurrent modes of treatment and have noted how their patients are enjoying them. Since January of 2019 we can see a significant shift to adding multi-patient treatment programming across several affiliated companies. The chart below shows a steady increase month-over-month for 2019.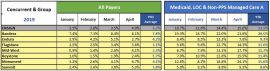
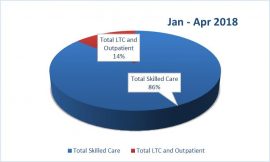
 Also, by providing multi-patient clinically appropriate treatment approaches, we create additional time to ensure we are providing care to our LTC residents and grow our outpatient programs. Note the trend from the first 4 months of 2018, to the first 4 months of 2019, as we increased our “Moments of Love” (Ciara Cox) for those that reside within our facilities and our communities from 14% to 19%!
Also, by providing multi-patient clinically appropriate treatment approaches, we create additional time to ensure we are providing care to our LTC residents and grow our outpatient programs. Note the trend from the first 4 months of 2018, to the first 4 months of 2019, as we increased our “Moments of Love” (Ciara Cox) for those that reside within our facilities and our communities from 14% to 19%!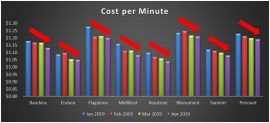
 Another area that would be great to study is the impact of Long Term Care therapy programming compared to changes in facility Quality metrics. Some markets already have been working on this and we would love to see your results!
Another area that would be great to study is the impact of Long Term Care therapy programming compared to changes in facility Quality metrics. Some markets already have been working on this and we would love to see your results! Pointe Meadows of Lehi, Utah uses the game, Headbands, in an SLP group. Headbands can be used to facilitate turn taking, processing speed, expressive communication, reading comprehension, and speech intelligibility
Pointe Meadows of Lehi, Utah uses the game, Headbands, in an SLP group. Headbands can be used to facilitate turn taking, processing speed, expressive communication, reading comprehension, and speech intelligibility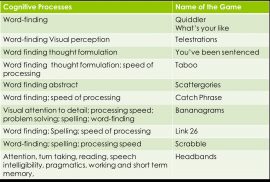

 world of greater creativity, compassion, and empathy, and strive to embody these traits in order to help others live happier, healthier lives.
world of greater creativity, compassion, and empathy, and strive to embody these traits in order to help others live happier, healthier lives.
 Essay by Cody Lemmons, DPT, University of St. Augustine, Austin, TX, Grad Date: 8/23/19
Essay by Cody Lemmons, DPT, University of St. Augustine, Austin, TX, Grad Date: 8/23/19

 Congratulations to our newest SPARC Award Winner, Jane Song! She is an Occupational Therapy student at Dominican University of California, and plans to graduate in May 2019.
Congratulations to our newest SPARC Award Winner, Jane Song! She is an Occupational Therapy student at Dominican University of California, and plans to graduate in May 2019.


