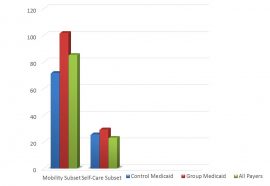
Occupational therapy and speech-language pathology co-treatment sessions provide comprehensive intervention and could fill a research gap on the benefits of this collaborative approach to advance patient outcomes in a SNF setting. Due to ever-changing and restrictive regulations, clear and effective documentation is necessary to ensure reimbursement and to expand the opportunities currently limited by billing protocols.
A review of current literature identifies information on the benefits of OT and SLP co-treatment sessions in a pediatric setting, but it fails to include outcomes of this collaboration in geriatric environments. The same hierarchy of skills addressed in the pediatric field often needs to be re-addressed as a natural part of the progression of aging. The skilled nursing facility presents multiple diagnoses impacting ADL/IADL performance, which could best be addressed by this underutilized interdisciplinary approach.
Literature Review
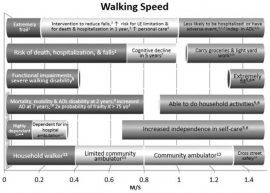
OT and SLP collaborations can provide comprehensive interventions during self-feeding, ADLs and general therapeutic activities. Planned meal-time co-treatments can include an OT assessment of wheelchair/seating positioning, ROM, strength and coordination for both hand-to-mouth and utensil manipulation, while an SLP assesses labial seal, oral motor control and other dysphagia concerns.
When an OT is providing skilled education and assistance to increase patients’ independence with ADLs, an SLP can assist by highlighting the necessary cognitive processes to complete the task and provide education and cues for improved carryover of learning.
This interdisciplinary support can also occur when IADLs and community reintegration are appropriate in a patient’s discharge plan. Additionally, increasing the cognitive demand and executive function components during therapeutic activities incorporating standing tolerance, dynamic balance, fine/gross motor coordination, safety, functional mobility and community needs can provide a more holistic approach to patient care (Ellenbaum, 2010).
Methods and Assessments
- Identify patients with varying diagnoses appropriate for skilled OT and SLP treatment
- Discuss treatment plan of each discipline and identify goals appropriate to address during scheduled co-treatment sessions
- Identify appropriate assessment tool/standardized measure to assess patient outcomes pre- and post-certification period with consistent co-treatment sessions
Potential OT Assessments
- Barthel Index
- Daily Activities Questionnaire
- Functional Assessment Scale
- Present Functioning Questionnaire
- Allen Cognitive Level Screening Assessments and Modules
- Safety Assessment of Function and the Environment for Rehabilitation (SAFER)
Potential SLP Assessments
- CLQT, MOCA-B, RIPA-G, SLUMS
- MASA, Bedside Swallow Evaluation, MBS/VFSE
- Determine the effectiveness of treatment interventions performed during reporting period including co-treatment sessions using pre- and post-test scores
- Compare pre- and post-test scores of patients with similar diagnoses not receiving co-treatment interventions
- Gather additional qualitative data using daily documentation of co-treatment sessions to determine effects more directly related to this approach
Intervention strategies include but are not limited to:
- ADL sessions
- PENS electrical stimulation protocols
- Therapeutic activities
- Community reintegration
- NMES electrical stimulation protocols
- Synchrony
- Meal assessment
- Diet texture analysis
Documentation
Co-treatment is not suitable for all residents. Therefore, the decision should be made on a case-by-case and even day-to-day basis and needs to be well-documented for each session (Ensign Services, 2016).
According to a joint position statement from AOTA, APTA and ASHA: “Co-treatment is appropriate when coordination between the two disciplines will benefit the patient, not simply for scheduling convenience. Documentation should clearly indicate the rationale for co-treatment and state the goals that will be addressed through this method of intervention.”
“Co-treatment sessions should be documented as such by each practitioner, stating which goals were addressed and the progress made. Co-treatment should be limited to two disciplines providing interventions during one treatment session” (Ensign Services, 2016).
Conclusions
Co-treatment sessions are intended to increase therapy intensity by cohesively targeting multiple goals with the same functional activity and an opportunity to provide increased services that may otherwise be limited by patient fatigue level or willingness to participate. Co-treatments are meant to be planned prior to scheduled treatment to highlight goals being addressed by each discipline and identify his/her role during the session.
A skilled need for a co-treatment approach should be identified before any treatment planning begins. Additionally, clear and effective documentation is the key for conveying the insight and skilled need for providing this service.
By Stacia Kozidis, OTR/L & Caitlin Timmins, MA, CCC-SLP, Clarion Wellness and Rehabilitation Center, Ensign Group & HCR Manor Care Waterloo


 Consider the following patient profile: A 19-year-old with traumatic brain injury secondary to assault presented with moderate deficits in immediate and short-term memory as well as temporal and spatial orientation. He was also legally blind as a result of his injury.
Consider the following patient profile: A 19-year-old with traumatic brain injury secondary to assault presented with moderate deficits in immediate and short-term memory as well as temporal and spatial orientation. He was also legally blind as a result of his injury.