Emergency Fund Spotlight
Congratulations to our SPARC winners (Corinne McGownd) and runner-up (Colleen Fitzgerald)! The judges felt their awesome essays below demonstrated they were both very special people.

My grandparents are in their late 80s and every day I am able to witness them show their love to each other as well as to others. Over the years, my grandparents have taught me compassion, putting others first, and being able to laugh even when things aren’t going my way. Everyone has something to teach no matter their age, cognition level, or disability. It is important to create an environment that provides people the ability to show their strengths while maintaining a positive attitude in order to increase their quality of life. When I am able to start practicing speech pathology, I plan on using my passion for helping others and learning to aid in increasing patient’s well-being in all aspects of their lives.
The most important thing I have learned from my academic coursework is to assess and treat patients with regards to their whole person and not to the disability. Speech therapists are treating the whole person during therapy, not just the disability; therefore, that is how assessment and treatment should be set up. I have seen this action while at my clinical practicum sites over the past year. I am currently at a specialty school for children on the autism spectrum. Although this is not a skilled nursing facility, I believe that these concepts can be transferred to any setting. At the school I am working in, the interdisciplinary care meetings about the each student are done on a regular basis. As a representative of speech therapy, I do not just discuss the student’s speech therapy goals within the meeting, but how the student is doing overall when I see him or her: transitions, overall attitudes, the conversations we have that don’t revolve around speech, and the generalization of what we are working on to other areas of the student’s schooling. The main goal of those meetings are to assess where the student is and how the team can best fit the needs of the student to improve his or her overall school experience.
Now translating this to a skilled nursing facility, I hope to be able to take an interdisciplinary approach by focusing on how the team can best increase the patient’s quality of life in all areas. Instead of simply working on word finding with the patient only in the context of their room, for example, speech therapy could focus on word finding in everyday activities: dining hall, getting dressed, communicating with nurses and family, or participating in desired activities. By working with other therapies and professionals, I will be able to assist the others on the team to provide best care for the patient that extends beyond the therapy room. Working on an interdisciplinary team also requires learning. I am eager to learn from my colleagues about best practice in their specialties and individualized patient care in regards to a specific patient in order to treat the whole person. Interdisciplinary care meetings would not be beneficial for the patient if there was no learning involved between the professionals. By learning from others, all professionals will be on the same page as well being able to provide the best care for the patient as possible.
In addition to learning from professionals, I envision myself learning from the patient themselves in order to contribute to their well-being. In order to provide patient centered care, it is important to learn what the patient wants to accomplish, what their abilities are, and what they are interested in. For example, my grandmother really enjoys playing golf. If I were to do speech and language therapy, I would want to learn from her about the difficulties she may be having when golfing in relation to her communication. By working on those things to increase her golf experience, whether that be socializing with the other players or being able to keep score, her quality of life in regards to her activities will increase because I spent the time to listen and learn from my patient. In addition to learning from others, I envision myself being a life-long learner. Through my schooling, I have always been curious and gone the extra step to understand the why behind doing something. By understanding why a therapy technique works and who it best works for, I would ultimately be increasing the patient’s therapy successes because I would be able to use evidence based practice when designing therapy plans.
I was fortunate to attend the American Speech-Language-Hearing Association annual convention this past November. While there I witnesses professionals of all levels of experience learning from others. They all had the same goal in mind: to learn and take back the new evidence to incorporate into their therapies with their patients. What a wonderful experience to witness! People from all over the country with the same passion! By keeping up with the research and the new therapies, I will be able to provide the most updated evidence based practice to my patients.
Learning is a passion of mine. Throughout my childhood, my grandfather taught me how to play basketball and the dedication it took to develop a skill. My grandmother taught me how to play cards and the patience it takes to play with others. Throughout my academic career, my professors have taught me how to look at the whole patient and how to critically assess evidence. Throughout my clinical placements, my supervisors have taught me how to use compassion with every patient. My patients have taught me how to really listen and look at the big picture. I hope that I can take all of these life lessons over the years and apply them while working with my patients. Every opportunity presents with a learning experience. Whether that opportunity involves working with a patient, sitting in an interdisciplinary care meeting, or independent learning about a specific treatment technique. Being able to recognize what that experience is teaching me is the first step. Then being able to take that experience and apply it to future experiences is the important next step. Without applying what is learned, then no one benefits. Ultimately, the end goal is to enhance the well-being of every patient. With that goal in mind, learning is a must in order to assist that patient in what they need to contribute to their quality of life. I want to make a difference in every patient I work with. In order to do that, I need to listen and learn from the team members and their expertise, the patient and their desires, and the others in my field and the ever growing knowledge base they present with.

E.D. Nixon once wrote, “Your spark can become a flame and change everything.” As an occupational therapy student, I feel that this quote is important because as OT’s we enable our patients to light their spark in order to bring back meaning to their lives. Once we light that spark for our patients it opens many doors for them. This may give them the motivation to work towards their goals and get back to their normal lives. Throughout the therapy process we collaborate, using our knowledge and our patients needs and interests, to get them back to where they want to be in life.
For example, this past summer I was treating a patient during my fieldwork that was very down. She was not allowed to bear weight on her left leg because of a surgery that she just had. She was not motivated to get dressed in the morning or shower. I began to ask her about herself and what was important to her. She stated that she felt uncomfortable being in the therapy gym without makeup and did not feel like herself. I had her family bring in some of her makeup and scheduled her therapy in the morning. I would have her practice transferring to the sink and keeping weight on only her right leg as she applied her makeup. This was a more meaningful way of increasing her balance, strength, and endurance that she needed to complete her daily occupations. Incorporating something that she loved to do enabled her to recover.
Along with this experience, I had many more this past summer while on my first level II fieldwork at Health South Rehabilitation Hospital. I was able to see how I will be using my knowledge and education in the future to better patients and allow them to become independent. Really listening to patients and using your therapeutic use of self is a great way to get to know your patients when you first start to work with them. There were many cases that if I hadn’t taken my time to get to know the patient I would have never figured out what some of their barriers were to a safe and independent discharge. I feel that with my education and my upcoming fieldwork, that I will be able to understand patients and work with them to meet their goals in the future.
I feel that I was very fortunate to go away to good school, better my education, and get into a great OT program. These past few years, I have taken every opportunity that is placed in my path to improve upon myself and the care that I will be giving to my patients. Throughout my time as an OT student and my fieldwork experiences, I have learned that the most important thing is to be patient and create good rapport between you and your patients. Once you have a good relationship with the patient, they will trust you and open up about other troubles or barriers that may be preventing them from reaching their goals. When working with patients, I feel that the three most important traits to have in order to become close with them and really understand what is going on in their lives is compassion, empathy, and patience. This will allow for your interventions to be holistic; meaning the physical, mental, and emotional aspects of the person are all taken into consideration.
One specific setting that I recently found interest in is the mental health and homeless population. This is considered non-traditional OT, but still views each patient holistically. I was fortunate enough to have one of my level one fieldwork’s at a mental health/homeless drop in facility in West Virginia. This experience really opened my eyes to the stigma that individuals with a mental health illness face. Every day we would complete some sort of art activity or have a music group to relax and then have a discussion group. Getting to know these individuals and help them work toward or reach their goals was something that really interested me. During my time at the facility, I was able to work with many individuals and figure out what I could leave them with that would best help them. I was able to put together a portfolio to assist them in getting a job, including things such as how to make a resume, what to bring to an interview, mock interview questions, how to manage money once getting a job, etc.
I am glad that I am already beginning to see the impact that I have made on some of the patients that I have worked with. I realized this almost immediately at each of my fieldworks. Seeing such amazing results before I even graduated was a great feeling. Knowing that I am able to help and possibly change someone’s life is very rewarding. Every day my passion for OT is growing and allowing me to learning new things. Along with my love for working with patients, I am very interested in reading articles regarding OT practice. Every night I try to research some of the newest information for evidence based practice. I try to do this because no matter what setting I am in I am going to get thrown in situations. Even if I am not an expert at something, having some knowledge about the situation can help. Finding this information and using it with my patients will allow me to give them the best care possible. Getting in a habit of doing this will increase my knowledge and quality of care for my patients.
As I watch each patient that I work with grow, I always think back to where my passion for OT started. When my younger cousin was born she was diagnosed with Down’s syndrome. She eventually began to receive OT and I would sit in on some of her sessions. I had to opportunity to watch how OT changed my cousin’s life and this was very inspiring. Her OT was extremely knowledgeable and humble throughout the entire process. I immediately aspired to be just like her. I began shadowing in multiple settings to see if I really did love OT. I continued to shadow for a few years and my love grew. I eventually got into WVU’s OT program and have continued to gain knowledge on how to help our patients. I can only hope that one day someone’s family has the same feelings towards me just like my family did for my cousin’s OT.
 The North Mountain Therapy Department specializes in Pulmonary Rehab, encouraging a multi-disciplinary approach to meet our respiratory patients’ goals of being decannulated, which typically is dependent upon the patient’s ability to return to a regular diet. In an effort to contribute to the greater independence of our patients, the Therapy Department created the SPOT (Speech Pathology Occupational Therapy), a holistic approach to a specialized dining experience to facilitate independence with safe swallow techniques and self-feeding.
The North Mountain Therapy Department specializes in Pulmonary Rehab, encouraging a multi-disciplinary approach to meet our respiratory patients’ goals of being decannulated, which typically is dependent upon the patient’s ability to return to a regular diet. In an effort to contribute to the greater independence of our patients, the Therapy Department created the SPOT (Speech Pathology Occupational Therapy), a holistic approach to a specialized dining experience to facilitate independence with safe swallow techniques and self-feeding.
The SPOT is a private, home-like, therapeutic dining room that allows our speech therapists and occupational therapists to provide a specialized treatment to our respiratory patients. The SPOT provides a quiet area to concentrate on safe swallow techniques, facilitate functional positioning, assess for any adaptive equipment needs to enhance the ability of our patients to regain their independence and return to the community.
The SPOT includes a small ADL kitchen and is stocked with adaptive equipment for the patients to trial during meals including a deltoid aid, weighted/built-up utensils, specialized drinking cups, and divided plates/plate guards. Additionally, ST has a quiet environment to perform vital stim or cognitive treatments.
The SPOT dining: helping North Mountain serve up independence!
Submitted by Kelly Schwarz, DOR
North Mountain Nursing & Rehabilitation, Phoenix, AZ
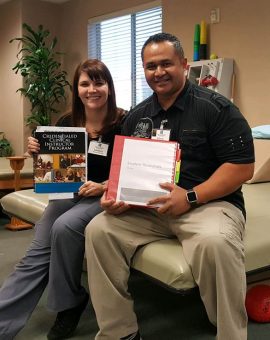 What was initially simply a continuing education experience for two therapists has inspired a brand-new program here at Coral Desert Rehabilitation. Recently, a Coral Desert physical therapist, Lindsay Rankin, and a physical therapist assistant, Edwin Stevenson, attended a course to become credentialed clinical instructors. They both enjoy having students, so they were excited to go. After attending the course, they came back with a desire not only to improve their own abilities, but also to help revamp the student program at Coral Desert.
What was initially simply a continuing education experience for two therapists has inspired a brand-new program here at Coral Desert Rehabilitation. Recently, a Coral Desert physical therapist, Lindsay Rankin, and a physical therapist assistant, Edwin Stevenson, attended a course to become credentialed clinical instructors. They both enjoy having students, so they were excited to go. After attending the course, they came back with a desire not only to improve their own abilities, but also to help revamp the student program at Coral Desert.
The program was loosely managed before and not standardized from one therapist to the next, so the students often had varied experiences and subjective learning/feedback depending on the therapist. Lindsay and Edwin decided to set a BHAG together to create and implement a better student program based on the principles and recommendations of the course they attended.
With a lot of after-hours work and trial and error with a current student, Lindsay and Edwin were able to create a student resource manual for the clinical instructor. This manual is specific to our building, patient population, etc. and loaded from A to Z with information on how to properly supervise a student of any discipline. They didn’t stop there. They also created a manual for each incoming student, both a PDF file to have prior to arriving and a hard copy for when they get here for reference.
Once both manuals were completed, after many rough drafts, it was presented to our therapy team during an in-service to give an in-depth look at how to use this information and apply it when a student is assigned to a therapist. This has already proved to be valuable with our current students and should continue to be a great resource for students and therapists for a long time to come. Because we have seen a steady increase in the number of students coming to CDR in the past two-plus years, it is just what we have needed since our therapists are at varying levels of experience with having students. We already have seven students committed to CDR from now until November of next year! We are crazy excited about the Passion for learning combined with Ownership shown by our own therapy team, which saw the need and responded in a big way.
Submitted by Asa Gardine, DOR, Coral Desert Rehabilitation, St. George, Utah
Congratulations Kristi Crozier, our Newest SPARC Winner!
Kristi is an OT student at Midwestern University in Glendale, AZ and will graduate in November 2017.
Read her awesome essay here:
As a wilderness therapy guide, I camped in the high desert with at-risk teenage students and taught outdoor survival skills. The most difficult and rewarding skill I taught was making matchless fires using bow drills. The process began by helping students search for the tools needed to create a spark: a straight stick and string for a bow drill, a flawless log for a fire board, dry grass for tinder, and a notched rock for a socket. Using these tools, the students learned the techniques to create fire and began to practice. The process was extremely challenging and weeks of bow drill practice typically yielded only bruised fingers and tears of frustration. However, the students’ frustration melted away when they were able to properly align their tools, find a rhythm, and persevere until they created heat, then smoke, and finally a tiny, glowing ember. Even the most reserved students celebrated and proudly proclaimed their accomplishment to the world when they created a spark. The creation of this spark was significant event and marked the first major step in each student’s journey of transformation and healing.
The creation of a spark, whether physical or metaphorical is a difficult process which yields great rewards. As an occupational therapist, I want to help my clients by creating sparks inside them that can generate blazing fires of achievement and wellness. I will use my knowledge and training from a rich variety of life experiences to help my clients by providing tools, knowledge, and support to ignite sparks of independence, understanding, and hope. Helping others has always been rewarding for me and I relish the satisfaction that comes from doing something for a person that they cannot do for themselves. However, I have learned through my training that the true purpose of therapy is not to help others by doing things for them, rather, it is to provide individuals with the tools they need to spark their own successes. I recently achieved this with a client during a clinical rotation. My client had a goal to live independently in her home but was challenged by a lack of active finger flexion which prevented her from grasping items. Using my training in orthotics and assistive devices, I fabricated a glove with a fastening system that could be strapped to tool handles. This glove enabled her to use both hands to complete cherished gardening and yardwork activities. When my client used this glove to hold a broom and sweep the floor of the therapy room, her eyes glowed with pride. The use of this simple tool allowed her to independently participate in an activity that she was unable to accomplish before and she was elated by her increased independence.
Using this physical tool generated a spark of independence and pride in my client. However, it was not the most effective tool I provided. The most important tool I provided was knowledge. As I worked with this client exploring ways to use the glove, we problem-solved modifications to overcome barriers to many of her occupations. Using basic principles of activity modification and assistive equipment, we identified ways to increase participation in various tasks. As we worked, I helped her to understand principles that she could employ in a variety of situations to facilitate her independence. She was a willing student and soon reported using her new knowledge to create adaptations at home. This knowledge created sparks of innovation and which will fuel her independence for the rest of her life.
The example above shows the power of a spark of knowledge, but before that spark can be used, it must first be acquired. To ignite sparks of knowledge in future clients, I plan to use a model I learned as a PATH therapeutic horseback riding instructor: the “what, why, how” model. First, clients must know “what” they are supposed to learn. This involves using language appropriate to the client’s understanding to explain an overview of the concept. Next, a client must be told “why” this concept is important. This step is imperative to ignite a client’s motivation and gain their trust. The final step is to teach “how”, which is to teach the actual concept in an organized, stepwise manner. This process is meant to shed light on the motivational and practical aspects surrounding a concept in order to help clients be more accepting of new knowledge and facilitate a deeper understanding.
This method of teaching was crucial when I taught a horseback riding class for students with high-functioning multiple sclerosis. I taught clients to perform physically and emotionally demanding tasks by explaining the task and providing a “big picture” of what was expected. Then I gained their trust and “buy in” by teaching them why the task was important and why it would improve their performance. And finally, I taught them the specific steps needed to achieve success. Using this method, I saw greater motivation for change in my students. When they understood what they needed to do, why they should do it, and how they could accomplish the task, they were more willing to listen and follow my recommendations. As a result, my students received sparks of understanding which erupted into success both in the riding arena and in their daily lives. I plan to continue using this method to generate sparks of understanding in my future clients and help them on their path to success.
Before I can ignite sparks of knowledge and understanding in my clients, I must first ensure that my own fires are fueled by actively seeking opportunities for professional development. This spring, I was a co-presenter at both the national American Occupational Therapy Association conference and the Assistive Technology Industry Association. These experiences fanned my flames of knowledge and fueled my enthusiasm for professional growth as an occupational therapist. At these conferences, I shared knowledge with other professionals and learned a great deal from them in turn. My mind was expanded by new ideas, innovative products, and novel research. This knowledge was indispensable during my clinical rotations and I was able to use the ember set aglow by my experiences to enlighten the minds of clients and therapists with whom I worked.
While knowledge and understanding are key elements of change, they are of little use without the spark of hope, a belief that something good can come from one’s efforts. Rehabilitation is a difficult process that takes great toll on clients. The physical and emotional strain can reduce a client’s spark of hope to smoldering embers. As a therapist, it is important to possess genuine concern and use therapeutic interactions to bolster the spirits of clients and rejuvenate their hopes. I witnessed the importance of rejuvenating a client’s sense of hope during my medical mission to Guatemala. The patients I saw struggled with injury and degeneration resulting from years of manual labor. These good people were in great physical pain and were weary of fighting their conditions. With limited resources and a limited knowledge of the Spanish language, it was difficult to find ways to ease their pain. However, I found that I could perform a great service by simply lending emotional support. Through listening and demonstrating concern, I bridged the communication barrier to connect with my patients and renew their sputtering flames of hope. Watching the darkness of despair dissipate as clients perceived my genuine concern and accepted my meager assistance was a powerful experience. I hope to continue that same level of concern and therapeutic connection to spark hope in my future clients. Armed with knowledge, training, and a genuine concern for my clients, I will be a catalyst for change in the lives of my future clients. Just as I helped my students in wilderness therapy create physical sparks, I will use my knowledge and training to ignite metaphorical sparks of independence, knowledge, and hope for my future clients. By providing tools, knowledge, and support I will set the therapy world ablaze.
 Clients with dementia living in skilled nursing facilities have occupational needs that are often unmet. Individualized care approaches and engagement in meaningful activities are effective non-pharmacologic approaches to dementia care. However, they are infrequently implemented in SNFs, and patients with dementia are often medicated with antipsychotic medications to manage behavioral symptoms related to dementia.
Clients with dementia living in skilled nursing facilities have occupational needs that are often unmet. Individualized care approaches and engagement in meaningful activities are effective non-pharmacologic approaches to dementia care. However, they are infrequently implemented in SNFs, and patients with dementia are often medicated with antipsychotic medications to manage behavioral symptoms related to dementia.
Occupational therapy practitioners and students who practice in SNFs may benefit from training to develop the knowledge, skills, attitudes and beliefs required to meet the unique occupational needs of clients with dementia who reside in long-term care SNF communities.
Background
Abilities Care Approach to Dementia:
Abilities Care Approach Process
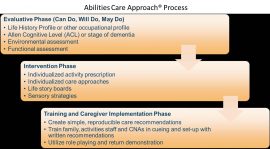
Implementation: Online Training Program
The online training program is available to OT practitioners and students through Ensign-affiliated SNFs. It incorporates effective teaching methods, including opportunities for student reflection, interaction with content, self-assessment of learning and application.
The training program is designed to:
Note that additional references and literature are available upon request for those interested in implementing the Abilities Care Approach to Dementia.
By Gina Tucker-Roghi, OTD, OTR/L, Therapy Resource, Northern CA
Urinary incontinence is a hidden epidemic. UI is among the 10 most common chronic conditions in the United States and is even more common than hypertension, depression or diabetes.
A majority of residents in skilled nursing facilities have some degree of incontinence. UI is quite costly in terms of quality of life of residents and the financial impact on facilities. As such, our Bladder Training Program seeks to address any incontinence issues among our residents.
Benefits of the program include:
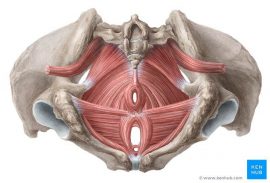
Pelvic Floor Muscles
Methods
Step 1: Patient identification — Review Quality Indicator report. Look for residents with “Urinary Incontinence.” There is correlation between UI and fall, so consider those who have fallen. Look at female patients with history of hysterectomy (there is a strong correlation between the procedure and UI).
Step 2: Nursing assessment — Identify type of incontinence, i.e., stress, urge, mixed, functional or overflow, by using incontinence assessment form and simple three-day voiding diary:
Step 3: Therapy evaluation — Stress, urge and mixed are the most common types to address by therapy intervention. Develop four-week pelvic muscle exercise (PME) training program.
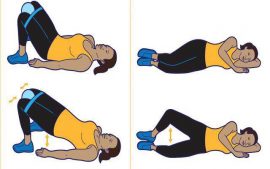
Step 4: Four-week treatment — PMEs to improve the strength and tone of pelvic floor and related muscles to maintain continence. PMEs include Kegel exercises, hip adductor exercises, obturator internus/abductor exercises, transverse abdominal exercises and gluteal sets.
Step 5: Re-evaluation — With improvement in urinary incontinence after four weeks of trial of PMEs, patient d/c from program. If no significant improvement in UI after four weeks of PMEs, electric stimulation and/or biofeedback is indicated, followed by reassessment.
By Kumar Pradeep, DPT, DOR, Legend Oaks Healthcare and Rehabilitation, South San Antonio, TX
 After noticing a recent increase in falls and fall-related injuries at our building, we wanted to better understand the mechanisms of the falls and implement a comprehensive, interdisciplinary fall prevention program.
After noticing a recent increase in falls and fall-related injuries at our building, we wanted to better understand the mechanisms of the falls and implement a comprehensive, interdisciplinary fall prevention program.
Consider the following data:
*Repeat offenders refers to residents who sustained more than one fall in a one-month span
What is the Falling Leaf Program?
This program was developed by Carolyn Spradlin as an adaptation to the Falling Star Program. The identified problem with the Falling Star Program is that it identifies patients at any risk of falls and results in a large number of patients in the program, thus decreasing the effectiveness.
In contrast, the Falling Leaf Program identifies the residents who are at the highest risk of falls. The program works to monitor these specific residents and determine the underlying reasons for these falls. A visual symbol of a leaf is placed outside the patient’s door and is used as a way for team members to intervene more quickly and better meet their needs.
How is it implemented:
Initial Findings
Results After One Month of Program 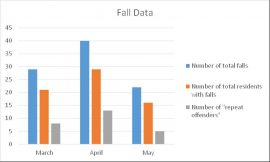
Conclusion
The implementation of this program at our facility is still in its early stages as we continue to work out any issues that arise. Some of our initial future plans include weekly reviews to assess for residents who can be removed from the program as well as any additional identified high-fall-risk residents who need to be added to the program. Additionally, we have recently started involving our pharmacy representative in fall meetings to assist with medication reviews to further decrease potential falls.
By Nicole Veniegas, DOR, MS, OTR/L; Kathryn Case, MOT, OTR/L, Magnolia Post Acute Care, El Cajon, CA
View full poster here: Falling Leaf – Magnolia
 As healthcare professionals, we often discuss dementia in the context of various stages, that is, how far a person’s dementia has progressed. Sometimes, we’ll define a person’s stage simply as early-stage, middle-stage or late-stage; however, to be more exact, we use the Global Deterioration Scale (GDS), which assigns seven different dementia stages based on the degree of cognitive decline.
As healthcare professionals, we often discuss dementia in the context of various stages, that is, how far a person’s dementia has progressed. Sometimes, we’ll define a person’s stage simply as early-stage, middle-stage or late-stage; however, to be more exact, we use the Global Deterioration Scale (GDS), which assigns seven different dementia stages based on the degree of cognitive decline.
Below, we’ve provided an overview of these stages, along with appropriate activities for the resident. You’ll see that the stages progress from pre-dementia through the final stages when a patient requires much greater assistance.
Stage 1
Stage 2
Stage 3
Stage 4
Appropriate activities: games, cooking axs, puzzles, crafts, bingo
Stage 5
Appropriate activities: crafts, gross motor games, puzzles, sorting tools, stuffing envelopes, bingo, coloring, painting, baking and cooking, sorting and matching, sing songs, counting exercises, sorting and folding clothes, setting the table
Stage 6
Appropriate activities: same as stage 5 but with greater amount of cueing, scrapbooks, photo albums, busy boxes, reminiscing. May push objects such as mops or brooms, parachute, may hit or kick a target, dusting, washing tables, stirring juice or batter
Stage 7
Appropriate activities: tactile stimulation, music, drumming, reminiscing, roll golf ball, sitting and head control during axs, kneed bread dough, take out raisins, husk corn and remove silk, pudding painting
The GDS provides a precise means of identifying a patient’s degree of cognitive decline. By defining a patient’s disease stage, we can determine the best treatment approaches and facilitate good communication between patients and caregivers.
By Amber Howard, DOR, Legend Oaks Healthcare and Rehabilitation, North Austin, TX
 Last year, Ensign therapists were introduced to a new balance pad system called the Sanddune Stepper. It is said to have significant effects on improving proprioception and ankle strategy in patients with a neurological diagnosis.
Last year, Ensign therapists were introduced to a new balance pad system called the Sanddune Stepper. It is said to have significant effects on improving proprioception and ankle strategy in patients with a neurological diagnosis.
The device is constructed of a combination of memory foam and closed cell foam, which causes a rapid rebound of the memory foam, increasing the challenge and resistance with each step. This also equalizes the reaction force on the feet when the patient is standing, making the device respond closer to the patient environment.
Clinical Observations
How well does the Sanddune Stepper improve proprioception and ankle strategy compared to other balance pads on the market? The main difference between the Sanddune Stepper and other balance pads is the different type of foam allowing for rapid stepping and the division between sides (giving the device the sand dune look). This division allows the contralateral foot to be lifted with no effect on the other, because it is essentially two pads in one.
Evidence states that muscle fatigue in lower extremities is a contributing factor to reduced postural control (Fox et al). “Balance exercises comprising steady-state and reactive components should be included in a balance program with the goal to prevent elderly people from falling,” according to Granacher, Muehlbauer and Gruber.
Using the “running in place or flutter step” exercise suggested by the manufacturer, we see a rapid onset of fatigue in our patients and use this technique to improve resistance to fatigue. Using this device with patients diagnosed with Parkinson’s disease, we observe immediate carryover in most cases following three minutes of rapid stepping on the device. The patient will usually demonstrate better stepping with gait on firm surfaces following this treatment intervention.
In patients with medical diagnosis of stroke and related balance deficits, this device improves carryover of ankle strategy from the Sanddune Stepper compared to other foam balance pads and on firm surfaces. Bird et al states that learned response with balance training improves carryover through leg strength and balance training. This can have a positive effect on fall prevention in older adults.
Conclusion
At Olympia Transitional Care and Rehabilitation, we have been using the Sanddune Stepper as our go-to balance pad. We consistently see more rapid recovery in proprioception and ankle strategy with our neurologically involved patients.
There is still evidence to be collected and more case studies to be written. Our initial observation is that this device is a power tool in our arsenal of balance training devices, and we use it more frequently than our other balance pads. We suggest that a dedicated study on the effects of the Sanddune Stepper would be beneficial to the field of rehabilitation for our neurological patients.
By C. Scott Hollander, DPT, Olympia Transitional Care and Rehabilitation, Olympia, WA