Submitted by Sunny Chahal, PT/DOR, Eastview Healthcare and Rehabilitation, Houston, TX
Sanikqu Maire became our Interim DON in March 2021. She had gained experience in our sister facility at Legend Oaks Northwest as an ADON prior to stepping into a DOR role at Eastview. Late in May, she transitioned from an LVN to an RN and stepped into the DON position on a full-time basis. With little experience at the building or as a DON, she helped lead the building through our annual state survey in April2021 with only two minor deficiencies. With the state survey and MSCA completed, the big 5 at our building decided on some initiatives and goals for the building for the rest of the year. One thing that Sanikqa really pushed was to get our facility name and face more visible in our community.
Since March 2020, due to the COVID pandemic, our building had been largely in lockdown and restricted for visitation from resident families and the surrounding community. In 2021, we wanted to get out and reestablish and develop our ties into the surrounding East Houston area. In addition, one of our goals for 2021 was to develop an outpatient program where we could follow our discharged skilled residents and also look to develop relationships with assisted living facilities (ALFs) and independent living facilities (ILFs) where we could partner up and offer our services to the residents.
We have targeted three large ILFs within a 5-mile radius of the building, and have already set up and completed health fairs at two of those three facilities. At the career fair, we have representatives from the Admission/Marketing, Dietary/Nutritionist, Nursing, and Therapy present at separate booths. For two hours, residents from the facilities go booth to booth to perform screens and receive education.

At the dietary and nutritionist booth, the residents were educated on proper foods to eat and other preventative health tips. Next they would go to the Nursing section and get their blood pressure and O2 saturation readings. After that, they would go to the Therapy booth, where they would get their height/weight and BMI calculated. They would also do a single limb stance test and test their grip strength. They would be educated about our new mobile outpatient program and screens performed.
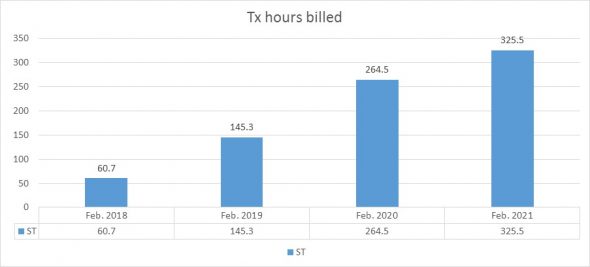
It was a success, as we obtained four to five therapy referrals from each career fair we completed. We have since gone on to exponentially grow our outpatient program over the past three months. Sanikqa’s energy and vision for community outreach and willingness to partner with Therapy and other departments in the building has been very instrumental to the success of our mobile outpatient program.