 As part of the Abilities Care Approach to Dementia, the SLPs in Northern Pioneers are working to create a specialty program to better assess pain in people with dementia. The Northern Pioneers’ facilities are triggering high in the Quality Measures of pain management for long- and short-stay residents. Recently, the cluster SLPs held a skills workshop on the use of a standardized test to support this work: the FLCI, or Functional Linguistic Communication Inventory. Park View Post Acute’s Director of Rehabilitation, Jennifer Raymond, is leading this pilot program.
As part of the Abilities Care Approach to Dementia, the SLPs in Northern Pioneers are working to create a specialty program to better assess pain in people with dementia. The Northern Pioneers’ facilities are triggering high in the Quality Measures of pain management for long- and short-stay residents. Recently, the cluster SLPs held a skills workshop on the use of a standardized test to support this work: the FLCI, or Functional Linguistic Communication Inventory. Park View Post Acute’s Director of Rehabilitation, Jennifer Raymond, is leading this pilot program.
Overview of the Communication of Pain (COP) Assessment
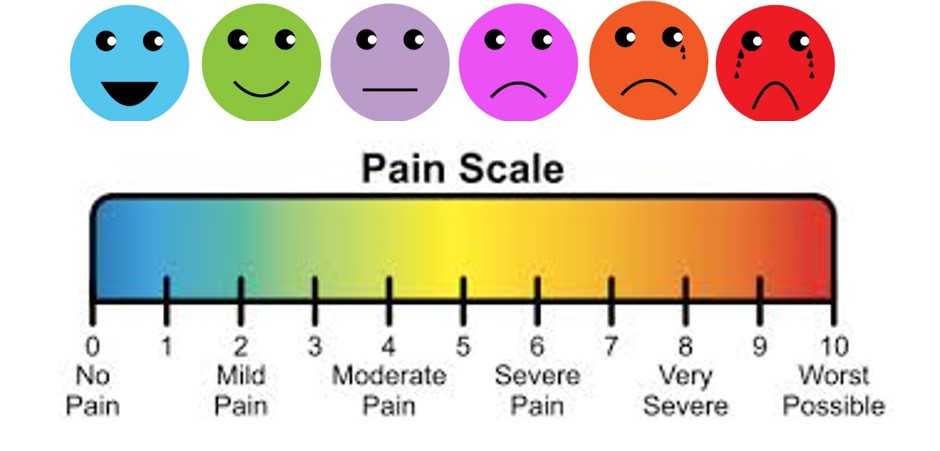
The SLP program is designed as an adjunct to Abilities Care for residents with cognitive and/or communication deficits who cannot utilize the “Tell me your level of pain on a 1-10 scale” system. Referrals occur through pain committee, behavior and psychotropic committee, Abilities Care programming and Quality Measures. The program uses FLCI standardized testing to establish a patient’s communicative ability and strengths. The therapist works with the resident to establish the most effective pain scale tool that utilizes remaining abilities: reading words; ability to point; auditory comprehension at the word, phrase or sentence level; visual scanning/tracking; and verbalization. A variety of scales are available, organized in a “toolkit” and sent out by Therapy Resource Tamala Sammons. Once a successful method/scale is identified, training is completed with the charge nurse and CNAs. Nursing Care plans an individualized pain communication system, which is then used by all staff with that resident.
Research shows that negative and difficult behaviors in persons with dementia are often expressions of unmet needs that they are unable to communicate. Pain is a primary trigger for negative behavior. The pilot program is a great way for therapy to support the facility in reaching its quality-of-care goals for all residents.
By Jennifer Raymond, DOR, Park View Post Acute Care, Santa Rosa, CA