Urinary incontinence is a hidden epidemic. UI is among the 10 most common chronic conditions in the United States and is even more common than hypertension, depression or diabetes.
A majority of residents in skilled nursing facilities have some degree of incontinence. UI is quite costly in terms of quality of life of residents and the financial impact on facilities. As such, our Bladder Training Program seeks to address any incontinence issues among our residents.
Benefits of the program include:
- Improves residents’ quality of life
- Improves quality measures
- Decreases the risk of pressure ulcers
- Decreases the cost of UI care (the direct cost of UI care is greater than the cost of breast, cervical, uterine and ovarian cancers combined, to the tune of an estimated $12.4 billion annually)
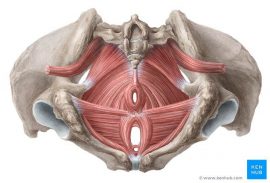
Pelvic Floor Muscles
- Pelvic Diaphragm: Levator ani muscle (Puborectalis, Pubococcygeus, Iliococcygeus) and Coccygeus muscles
- Urogenital Diaphragm: Deep transfer perineal, Sphincter urethrae
- Sphincters and erectile muscles of urogenital and intestinal tract: External anal sphincter, Bulbospongious, Ischiocavernosus, superficial transverse perineal
Methods
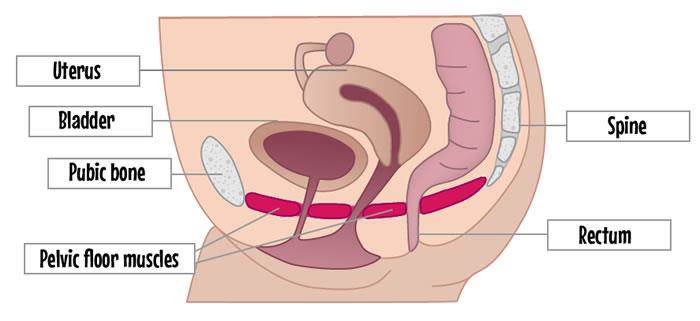
Step 1: Patient identification — Review Quality Indicator report. Look for residents with “Urinary Incontinence.” There is correlation between UI and fall, so consider those who have fallen. Look at female patients with history of hysterectomy (there is a strong correlation between the procedure and UI).
Step 2: Nursing assessment — Identify type of incontinence, i.e., stress, urge, mixed, functional or overflow, by using incontinence assessment form and simple three-day voiding diary:
- Stress type: Leakage of small amount of urine during physical movement, usually from pelvic floor muscle weakness.
- Urge type: Involuntary loss of urine associated with a strong desire to void. Leakage of large amounts of urine at unexpected times, including sleep. Sensory loss is a strong influence.
- Mixed type: Occurrence of stress and urge together. This is the most common type in the elderly.
- Functional type: Incontinence resulting from inability to access toilet due to physical disability, weakness, external obstacles, inability to manage clothing and/or cognitive impairment.
- Overflow type: Unexpected leakage of small amounts of urine (without movement) because bladder is excessively full due to damaged bladder, obstructed urethra or nerve damage.
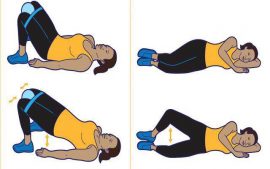
Step 3: Therapy evaluation — Stress, urge and mixed are the most common types to address by therapy intervention. Develop four-week pelvic muscle exercise (PME) training program.
Step 4: Four-week treatment — PMEs to improve the strength and tone of pelvic floor and related muscles to maintain continence. PMEs include Kegel exercises, hip adductor exercises, obturator internus/abductor exercises, transverse abdominal exercises and gluteal sets.
Step 5: Re-evaluation — With improvement in urinary incontinence after four weeks of trial of PMEs, patient d/c from program. If no significant improvement in UI after four weeks of PMEs, electric stimulation and/or biofeedback is indicated, followed by reassessment.
By Kumar Pradeep, DPT, DOR, Legend Oaks Healthcare and Rehabilitation, South San Antonio, TX


 After noticing a recent increase in falls and fall-related injuries at our building, we wanted to better understand the mechanisms of the falls and implement a comprehensive, interdisciplinary fall prevention program.
After noticing a recent increase in falls and fall-related injuries at our building, we wanted to better understand the mechanisms of the falls and implement a comprehensive, interdisciplinary fall prevention program.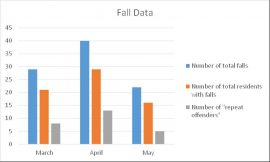

 At Grand Terrace Rehabilitation and Nursing, we have implemented an Oral Hygiene Program with great success for residents. The purpose of the program is multifold:
At Grand Terrace Rehabilitation and Nursing, we have implemented an Oral Hygiene Program with great success for residents. The purpose of the program is multifold:
 As healthcare professionals, we often discuss dementia in the context of various stages, that is, how far a person’s dementia has progressed. Sometimes, we’ll define a person’s stage simply as early-stage, middle-stage or late-stage; however, to be more exact, we use the Global Deterioration Scale (GDS), which assigns seven different dementia stages based on the degree of cognitive decline.
As healthcare professionals, we often discuss dementia in the context of various stages, that is, how far a person’s dementia has progressed. Sometimes, we’ll define a person’s stage simply as early-stage, middle-stage or late-stage; however, to be more exact, we use the Global Deterioration Scale (GDS), which assigns seven different dementia stages based on the degree of cognitive decline. Our skilled population has gradually shifted from traditional Medicare Part A to Managed Care Part A. Therefore, our treatment focus has had to shift as well. We are no longer focusing on progressing to prior level of function, but rather progressing to next level of care.
Our skilled population has gradually shifted from traditional Medicare Part A to Managed Care Part A. Therefore, our treatment focus has had to shift as well. We are no longer focusing on progressing to prior level of function, but rather progressing to next level of care. Last year, Ensign therapists were introduced to a new balance pad system called the Sanddune Stepper. It is said to have significant effects on improving proprioception and ankle strategy in patients with a neurological diagnosis.
Last year, Ensign therapists were introduced to a new balance pad system called the Sanddune Stepper. It is said to have significant effects on improving proprioception and ankle strategy in patients with a neurological diagnosis.
 Using the Life History and Profile, OT was able to identify purposeful and meaningful activities the resident enjoyed, including:
Using the Life History and Profile, OT was able to identify purposeful and meaningful activities the resident enjoyed, including: