By Evette Ramirez, PT, DPT, Keystone Therapy Resource/DOR Legend Oaks, Waxahachie, TX
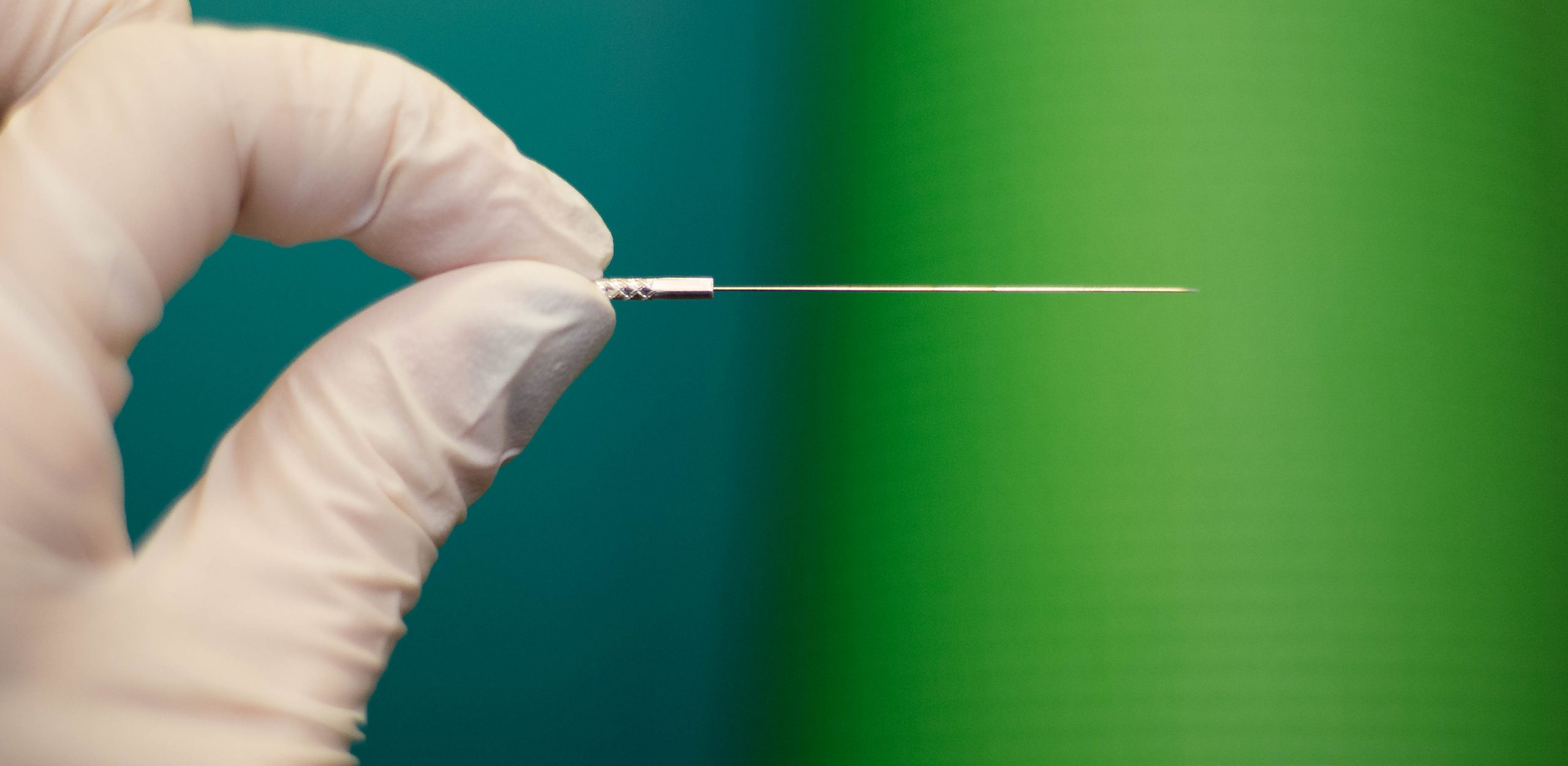
 Dry needling is a technique that has many uses, although it is often confused with acupuncture, which follows the principles of Chinese medicine. Dry needling is a technique in which varying lengths and gauges of acupuncture needles are used at nerve roots, nerve pathways, homeostatic points, muscle bellies, scars and/or the area of motor endplates as treatment areas.
Dry needling is a technique that has many uses, although it is often confused with acupuncture, which follows the principles of Chinese medicine. Dry needling is a technique in which varying lengths and gauges of acupuncture needles are used at nerve roots, nerve pathways, homeostatic points, muscle bellies, scars and/or the area of motor endplates as treatment areas.
The dry needling technique follows the rules and knowledge of the human anatomy and has a background derived from traditional medicine. It has been shown to help promote physiological homeostasis and allow the body to maximize self-healing of soft tissue dysfunction by creating a small lesion in the tissue, triggering an inflammatory process and healing. Dry needling should be practiced by a clinician who has had thorough training in needling techniques, has a strong knowledge of the human anatomy, and knows and understands precautions and contraindications so as to avoid doing harm.
Mr. A is a 76-year-old male who has had chronic pain for years. Years before coming to reside in our facility, he was treated by a pain management doctor for chronic pain in his back with radicular pain radiating into his bilateral quads. Our client was treated unsuccessfully for his pain. He also had a stimulator implanted, which he also reports did not help. This stimulator stopped functioning years ago when the battery ran down. He reports he has been unsuccessful in convincing any surgeons to remove it.
Due to his chronic condition, he came to reside with us at Legend Oaks of Waxahachie. At the time, he was not able to ambulate without assistance and the use of a walker. His condition continued to deteriorate, and walking became more and more difficult. His pain became so unbearable that he was having trouble sleeping. Functional transfers were difficult, and he began to develop muscle tightness in the bilateral hamstrings.
Mr. A received rehab services and made some progress, but he would begin declining once rehab services were discontinued due to a plateau in progress. Intermittently, there were complaints of hand pain, spasms and tightness, which was also treated. Along with these complications, he had a diagnosis of Parkinson’s, which was also progressing, and a neurology consult was acquired to assist with medication management and monitoring for progressively worsening tremors.
After I took the dry needling course through Integrative Dry Needling, he was the first person I wanted to work on. I explained to him what I wanted to do, which would be to start with his primary problem area. I placed him on the treatment table in a side-lying position and palpated his lumbar spine. I explained to him what to expect as far as sensation during the needling. I palpated L5 and the PSIS. Two finger’s width distance laterally from the spinous process of L5 is where I placed the guide, angled toward the spine, and inserted the 2-inch needle.
I did this bilaterally, inserting the needle until I felt the needle reach a bony barrier. As the needle was being inserted, I felt resistance. The sensation felt like rigid barriers being crossed. I described the sensation as feeling like pushing a needle through layers of paper — feeling resistance, then a slight “pop” and then free movement of the needle until the next layer was reached. I did this from L5–L3, bilaterally. He had an area at T12 that was also a problem area and was flared up that day. I inserted a 1-inch needle at that level, 1 inch from the spinous process, angled toward the spine. This was done as an “in-out” procedure. I inserted each needle until I felt a bony barrier. The entire treatment only took a few minutes and he reported only a mild ache at L5. He then completed the rest of his PT session for strengthening, manual stretch to B lower extremities progressing to WB activities.
The next day, our client’s roommate came to us and told us to keep doing whatever we did to his roommate because it was the best sleep either has had in a long time. He explained that typically, whenever Mr. A would even roll over in bed, he would call out in pain. Mr. A then came into the therapy gym with the biggest smile on his face. He said that within hours, his pain had decreased from a reported 8/10 to 4/10 and he hadn’t felt so little pain in years. He also reported having had a full night of sleep, and reported he could not remember the last time he felt so rested. We continued needling twice a week, primarily along these same areas.
The next week, our client was feeling much better where the back pain was concerned, but he was still having leg and quad pain. Along with needling his back, I added needling to the bilateral quads, hamstrings and IT bands with a 2-inch needle, again using the in-out technique. He reported feeling the needle on his quads during the needling but no other sensations. He then proceeded with his PT session.
The next day, he reported a decrease in quad pain, and the PT who was working with him reported improved ROM in knee extension bilaterally with manual stretch (as well as improved tolerance), improved standing tolerance and ability to stand more erect.
As he continued to receive PT services, he had a flare-up of hand pain and cramping. Pain was reportedly increased while maneuvering his wheelchair throughout the facility. In the past, OT had worked with him and had even attempted splinting with some improvement in pain level, but none of the relief would last once OT services had ended.
By this time, one of my staff PTs had also been trained in needling by IDN and asked him if he would allow her to needle his hands. He agreed to try because of the success with decreasing his back and radicular pain. She chose to needle at two homeostatic points in the bilateral UE. She needled at the deep and superficial radial points, which are along the path of the radial nerve. She needled at the forearm, distal to the radial head, then in the trigger point in the muscle between the thumb and forefinger, the dorsal interosseous muscle. This trigger point is also one that you will often hear of people pressing to relieve headaches and other pains.
He had an immediate reaction, with an extreme sense of euphoria and relief of the pain in his hands. He was kept in the therapy gym for monitoring, as we had not experienced anyone with this type of reaction. His vital signs were all within normal limits. Within a few minutes, he was back to feeling “normal,” and the pain in his hands had gone from 8-9/10 to a 4-5/10.
Mr. A has progressed so that he is off of routine pain medications and now takes them only PRN, when he has a flare-up. He continues to increase in function, with decreased pain at rest and with activity. ROM and coordination as well as tolerance to standing and ambulation continue to improve. We are working to lengthen the time he can go between needling sessions, and he is on more of a maintenance program for needling and pain management.