By Therapy Resources Brian Del Poso, OTR/L, CHC, RAC-CT and Jon Anderson, PT
In our last article (check out it out here), we talked about taking care of ourselves while we are adhering to Shelter in Place rules and fitness facilities are closed. Now I know we want to be optimistic about the beginning phases of re-opening businesses in our areas, but we, more than anyone else, are aware of the fight we still have ahead of us. So, let’s continue to stay active at home and be smart about social distancing with outdoor activity.
Let’s face it, with the challenges working in today’s era of COVID-19 healthcare, the amount of heart, physicality and emotion you pour out during a work day can get downright exhausting! This is why more than ever, even if exercising isn’t your thing, we encourage you to start and take care of your bodies … so if and when the time comes, your body will take care of you!
Previously, we focused on body weight exercises, but I know that might get old fast with some of you and you’d like some variety! Today we’ll provide some simple equipment ideas that you can DIY at home to take your workouts to the next level!
Slosh Pipe:
This is a 4 to 5 foot pipe filled halfway with water (1 gallon of water = about 8.3 lbs). The movement of the water creates an “unstable” weight. Performing movements using a slosh pipe will get your nervous system firing like crazy as you try to balance and stabilize the pipe while performing movements! Pro Tip: After you try it, think of the possibilities and effect a smaller version of this can have on neuromuscular re-ed for our patients!
How to make:
o Things you’ll need: 3 or 4 inch diameter PVC pipe, PVC pipe caps, and PVC glue from any big box home improvement store; a saw.
o Cut the pipe down (you can use a hacksaw for this) to 4 or 5 feet in length.
o Follow the instructions for the PVC pipe glue and glue 1 cap to an end of the pipe.
o Fill the pipe up about halfway with water (obviously A greater diameter and length of pipe will provide more weight).
o Glue on the other cap and slosh away!
What can I do with it? A TON of stuff, but to start you can do:
o Back squats
o Front squats
o Overhead presses
o Bicep curls
o Lunges
o Chest press from floor
o Trunk rotation (trunk twists, pipe swings, single oar rowing motions, etc.)
Medicine Ball/Slam Ball:
This is great if you have broken or unused basketball or soccer balls laying around.
How to make:
o Things you’ll need: Basketball or soccer ball, sand, exact-o knife, a funnel, duct tape.
o Take your ball and cut about a 2-3 inch circle with an exact-o knife, but DON’T completely cut out the circle! Leave some room so it’s still connected, but you can lift up the “flap.” Alternatively, you can cut an “X” into the ball to create an opening.
o Stick your funnel in your opening and fill with sand to your desired weight.
o Take your duct tape and thoroughly wrap around the ball in multiple directions to seal off your opening.
Things you can do:
o Ball slams
o Ball tosses
o Russian twists
o Anything you’d normally do with a medicine ball!
Weighted Backpack: You don’t have to be a workout warrior to take advantage of the health benefits of resistance training. This one is easy, adding weighted resistance to something as simple as walking will increase your strength and endurance.
How to make:
o Things you’ll need: A backpack and anything you can stuff in it!
o Take your backpack and stuff it with things to make it heavier (cans, clothes, your wonderful leadership books) … Ummmm, yea, and that about sums it up.
Things you can do:
o Cinch it up tight to your body and pretty much do ANYTHING moving … ’nuff said.
Buckets:
Got a bucket or 2 lying around the house? Well, fill them up with stuff (like sand, or you know, those leadership books again) and get to work!
Things you can do:
o Farmer’s walks
o Single arm shoulder presses
o Biceps curls
o Overhead triceps extensions
o Bucket swings (kettlebell swings) — Just make sure you use a smaller bucket, preferably with a lid!
Here’s a great example of a bucket workout using a 5-gallon bucket from our very own Jon Anderson:
Squat Curl to Press: A full body exercise.
Push-up With Feet Elevated: Exercise focusing on the pectoralis major of the chest while increasing the load by elevating the feet.
Lateral Lunge with Curl: Combination exercise targeting lower body muscles in a lateral movement as well as the biceps.
Bent Over Low Row: Exercise focusing on the latissimus dorsi of the back.
Deadlift: Exercise focusing on the hamstrings and gluteus maximus of the lower body.
Chopper Raise: A full body exercise.
Close Grip Tricep Push-up: A push-up alternative that puts greater emphasis on the triceps.
Reverse Lunge with Torso Rotation: Lower body exercise that also challenges balance and core strength.
Back Extension: Exercise focusing on using the erector spinae for stabilization of the spine.
Alternating 1 Leg Deadlift: Exercise that provides an increased load to the hamstrings and gluteus maximus of the lower body because it is performed on a single leg, which also adds a balance challenge.
A variety of other exercises could also be added or substituted using a bucket. Regardless of the exercise, perform each movement with special attention to proper technique. If starting out, consider creating and using a moderate weight that does not jeopardize form and feels like an exertion rating of a 5-8 on a scale of 1-10. Start by performing 1-2 sets of 10-15 repetitions, and as fitness increases, add additional sets.

 Our amazing ADOR George Palin and his wife have been working tirelessly to provide the entire building (and a few to our sister buildings) with cloth masks, and they are now working on gowns to keep us all safe. Today the team wanted to say a special thank-you to him. One of our other amazing PTAs, Heidi Carmichael, thanked George for providing her with a more comfortable mask (pictured — you gotta laugh sometimes, right?) and read the following poem as a thank-you. I thought this is so true of George and so many others who are going above and beyond to take care of each other and our residents.
Our amazing ADOR George Palin and his wife have been working tirelessly to provide the entire building (and a few to our sister buildings) with cloth masks, and they are now working on gowns to keep us all safe. Today the team wanted to say a special thank-you to him. One of our other amazing PTAs, Heidi Carmichael, thanked George for providing her with a more comfortable mask (pictured — you gotta laugh sometimes, right?) and read the following poem as a thank-you. I thought this is so true of George and so many others who are going above and beyond to take care of each other and our residents.

 By Jared MacDonald, Operations Manager, City Creek Post Acute Care, Salt Lake City, UT
By Jared MacDonald, Operations Manager, City Creek Post Acute Care, Salt Lake City, UT
 Victoria Post Acute (VPAC) is one of the few skilled nursing facilities accepting COVID-19-positive residents from hospitals in San Diego and El Centro. Like other buildings with positive COVID cases, the beginning stage was certainly an upheaval from “normal” daily routines, as we were thrown into a world of unknowns with ever-changing directions and recommendations, coupled with fear. Schedules were slim, admissions were down, and stress was high. The rehab gym became a room with social distancing markers and a storage room. Hallways turned into PPE stations.
Victoria Post Acute (VPAC) is one of the few skilled nursing facilities accepting COVID-19-positive residents from hospitals in San Diego and El Centro. Like other buildings with positive COVID cases, the beginning stage was certainly an upheaval from “normal” daily routines, as we were thrown into a world of unknowns with ever-changing directions and recommendations, coupled with fear. Schedules were slim, admissions were down, and stress was high. The rehab gym became a room with social distancing markers and a storage room. Hallways turned into PPE stations. As the days and weeks pass, admissions are starting to return, PPE requirements are changing, and barrier placements are being removed. Through it all, VPAC has remained resilient and together. Despite the loss and havoc of the first few weeks, we’ve found reasons (many, many, many reasons) to smile and celebrate. We have celebrated resident successes/discharges, birthdays, a retirement (DON), bridal shower, nurses week/nursing home week, Tuesdays and each other. We have been able to celebrate a COVID-19-positive patient (the husband of one of our charge nurses) being discharged home, walking out hand in hand with his wife after a month of hospitalization/rehabilitation including intubation.
As the days and weeks pass, admissions are starting to return, PPE requirements are changing, and barrier placements are being removed. Through it all, VPAC has remained resilient and together. Despite the loss and havoc of the first few weeks, we’ve found reasons (many, many, many reasons) to smile and celebrate. We have celebrated resident successes/discharges, birthdays, a retirement (DON), bridal shower, nurses week/nursing home week, Tuesdays and each other. We have been able to celebrate a COVID-19-positive patient (the husband of one of our charge nurses) being discharged home, walking out hand in hand with his wife after a month of hospitalization/rehabilitation including intubation.

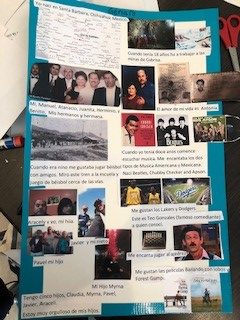
 Introducing Nicole King, one of our newest Directors of Rehabilitation at Ridgeview Post-Acute in Commerce City, Colorado.
Introducing Nicole King, one of our newest Directors of Rehabilitation at Ridgeview Post-Acute in Commerce City, Colorado.