It’s no news flash that walking requires quite a bit of lower-body strength. You need powerful glutes, quads, hamstrings and calves to propel you forward. You might also recognize the crucial role your abs play in keeping you upright and lightening the load on your lower half. But there’s one muscle you probably never even think about when it comes to your stride. We’re talking about your “lats” (or latissimus dorsi), the biggest muscle of your upper body. Affording itself a large attachment centrally from the T7 to L5 spinouses, laterally to the iliac crest and thoracolumbar fascia, to the lower three or four ribs and inferior angle of the scapula, to travel superiorly and laterally to attach to the medial lip of the intertubercular sulcus, it is perfectly situated to effect both the upper and lower extremities in a large variety of movements. It is one of the quintessential and often overlooked muscles in gait. It is generally quiet electrophysiologically (EMG) during pre-gait activities (1,2) but as speed increases, the muscle becomes more engaged and active (2-4). The latissimus dorsi is the functional link between the upper and lower extremity, particularly through its connections with the thoracolumbar fascia (5,6).
The lat muscle is a key driver in the Posterior Oblique Sling System, which helps explain the relationship between the arms and legs during the gait “walking” cycle. The posterior oblique sling is a cross-body pattern composed of the gluteus maximus, thoracolumbar fascia (TLF) and contralateral latissimus dorsi muscle, which connects the shoulder with the opposite hip to facilitate locomotion. Dysfunction in this system puts the brakes on power, strength, speed and performance. To understand how your lats affect your walking performance, think about your gait or your movement pattern while you walk: “As your left leg steps forward, your right arm swings forward, thus you’re creating a rotational force, the abdominals and lats help with this rotational movement. The stronger your lats, the easier this twisting motion becomes and the more efficiently you nail your stride. Plus, strong lats help ensure the rest of your muscles don’t have to work in overdrive. Translation: You won’t tire out so fast and you’ll be able to walk/jog/run for longer time frames. Whatever was fatiguing you before won’t fatigue as fast, because you’re bringing more muscles to the party. You’ll be surprised just how much your lats are a part of the equation once you focus on strengthening them.
An easy way to tell whether you need to increase your patient’s or perhaps even your own lat strength is to assess form. Here are a couple of tell-tale signs to look for when walking: If the patient/client starts to fall forward or slouch their head forward, and if the shoulder blades are creeping up by the ears, this most likely indicates an opportunity to strengthen the lats. But before you get started with those strengthening exercises, you need to make sure the surrounding muscles aren’t getting in the way, for example, tight triceps (the backside of the arm) or upper trapezius (where your shoulder meets your neck) can inhibit the lats from activating during exercises. This would work against the patient/clients best efforts. Once you have had the patient/client complete a few tricep and upper trap stretches, it’s time to start strengthening the lats. Some suggestions to start with include:
- Seated Row
● Using a resistance band or a cable row machine, sit upright with your legs out straight. If using a resistance band, hook it around your feet. No matter the equipment, roll your shoulders back and down, “packing” them into your lats.
● Keeping the elbows tight and close to your body, row your elbows straight back, pinching your shoulder blades together.
● Reset with control, then repeat.
● Do 3 sets of 10 to 15 reps. - Bent-Over Fly
● Stand with soft knees, holding a dumbbell in each hand by your sides. Hinge forward at the hips with a flat back and neutral neck. Allow your arms to hang down under your chin with a slight bend in the elbows.
● Leading with your elbows, bring your arms back and imagine you’re hugging a tree backward, squeezing your shoulder blades together. Hold for one second before lowering down with control.
● Do 3 sets of 10 to 12 reps with dumbbells appropriate for your patient/client. - Superman Lift
● Lie face-down on the floor with your arms and legs extended. Squeeze your glutes to glue your ankles together and lock your arms tight next to your ears. Keep your neck neutral, and gaze down toward the floor throughout the whole movement.
● Use your back to lift your legs off the ground, trying to lift your quads off the ground without bending at the knees. Lower with control. Repeat with just the upper body.
● Once you’ve mastered isolating the lower and upper, add them together, lifting all four extremities off the ground and holding at the top before lowering with control.
● Do 4 sets of 15 to 20 reps.
Beyond strengthening and stretching the lats to improve gait function, it’s also important to remember that if the patient/client has latissimus dorsi pain and/or referred pain, this can also impact range of motion and muscle activation patterns, including the patient’s gait quality. Dry needling is one modality that PTs may be able to use to decrease lat pain and improve the overall performance of this muscle by improving its function, thus improving range of motion and muscle activation patterns (7-9).
By Jon Anderson, DPT, Therapy Resource
References:
- Houglum P, Bertoti D in: Brunstrums Clinical Kinesiology 6th Edition, FA Davis 2012 p.558
- G. Cappellini, Y. P. Ivanenko, R. E. Poppele, F. Lacquaniti Motor Patterns in Human Walking and Running Journal of Neurophysiology Published 1 June 2006 Vol. 95 no. 6, 3426-3437 DOI: 10.1152/jn.00081.2006
- Shin S, Kim T, Yoo W. Effects of Various Gait Speeds on the Latissimus Dorsi and Gluteus Maximus Muscles Associated with the Posterior Oblique Sling System. Journal of Physical Therapy Science. 2013;25(11):1391-1392. doi:10.1589/jpts.25.1391.
- Kim T, Yoo W, An D, Oh J, Shin S. The Effects of Different Gait Speeds and Lower Arm Weight on the Activities of the Latissimus Dorsi, Gluteus Medius, and Gluteus Maximus Muscles. Journal of Physical Therapy Science. 2013;25(11):1483-1484. doi:10.1589/jpts.25.1483.
- Vleeming A, Pool-Goudzwaard AL, Stoeckart R, van Wingerden JP, Snijders CJ. The posterior layer of the thoracolumbar fascia. Its function in load transfer from spine to legs. Spine (Phila Pa 1976). 1995 Apr 1;20(7):753-8.
- Willard FH, Vleeming A, Schuenke MD, Danneels L, Schleip R. The thoracolumbar fascia:anatomy, function and clinical considerations. Journal of Anatomy. 2012;221(6):507-536.doi:10.1111/j.1469-7580.2012.01511.x.
- Dar G, Hicks GE. The immediate effect of dry needling on multifidus muscles function in healthy individuals. J Back Musculoskelet Rehabil. 2016 Apr 27;29(2):273-278.
- Ortega-Cebrian S, Luchini N, Whiteley R. Dry needling: Effects on activation and passive mechanical properties of the quadriceps, pain and range during late stage rehabilitation of ACL reconstructed patients.Phys Ther Sport. 2016 Sep;21:57-62. doi: 10.1016/j.ptsp.2016.02.001. Epub 2016 Feb 24.
- Dommerholt J. Dry needling — peripheral and central considerations. The Journal of Manual & Manipulative Therapy. 2011;19(4):223-227. doi:10.1179/106698111X13129729552065.





 Why is respiratory function so important for SLP involvement?
Why is respiratory function so important for SLP involvement?

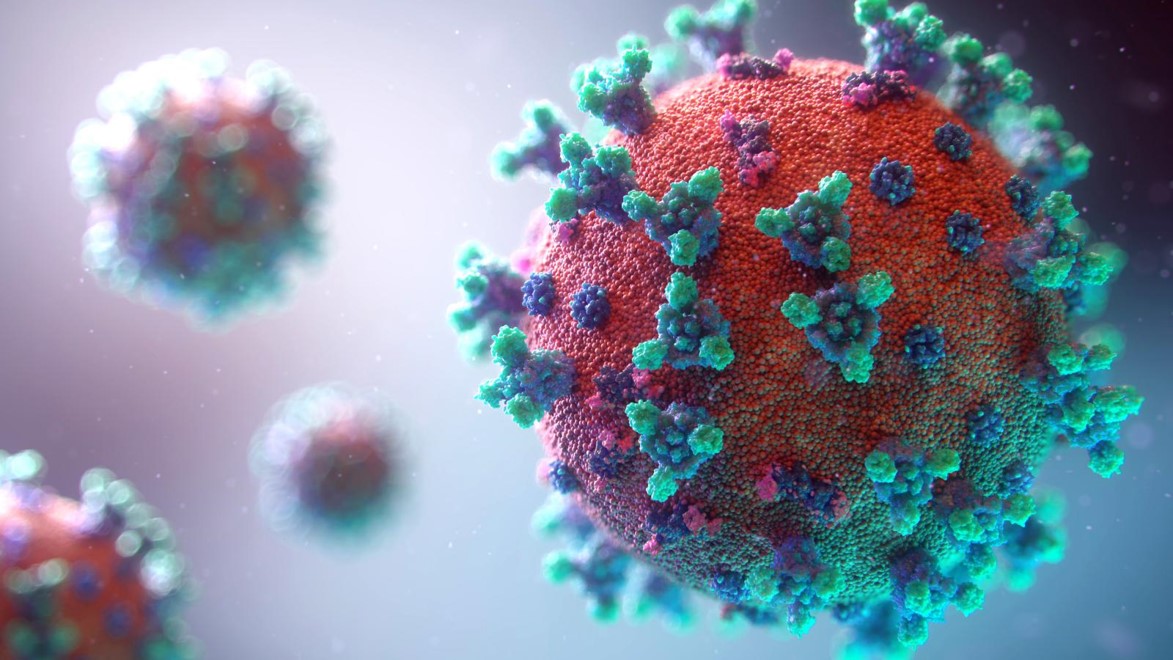
 COVID-19 is a respiratory viral disease with multi-organ involvement resulting in potentially temporary and episodic health challenges such as impaired lung function, physical deconditioning, cognitive impairments, impaired swallow and communication, and mental health disorders.
COVID-19 is a respiratory viral disease with multi-organ involvement resulting in potentially temporary and episodic health challenges such as impaired lung function, physical deconditioning, cognitive impairments, impaired swallow and communication, and mental health disorders.