By Tamala Sammons, MA, CCC/SLP, Therapy Resource
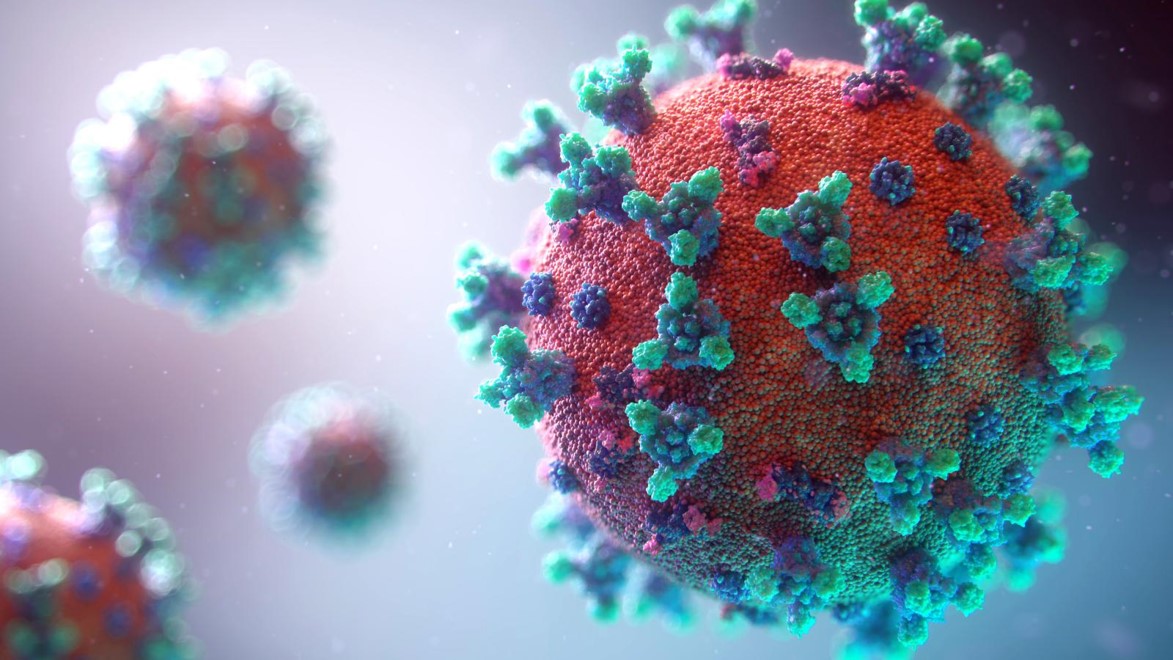
 COVID-19 is a respiratory viral disease with multi-organ involvement resulting in potentially temporary and episodic health challenges such as impaired lung function, physical deconditioning, cognitive impairments, impaired swallow and communication, and mental health disorders.
COVID-19 is a respiratory viral disease with multi-organ involvement resulting in potentially temporary and episodic health challenges such as impaired lung function, physical deconditioning, cognitive impairments, impaired swallow and communication, and mental health disorders.
The effect of the virus on the respiratory system appears to range from a simple respiratory tract infection to acute respiratory distress syndrome (ARDS) with multi-organ failure.
People with COVID-19 may also develop coagulopathy that can lead to venous thromboembolism (VTE) and microvascular thrombosis throughout the body, increasing the risk of negative mental health outcomes (https://academic.oup.com/ptj/article/100/12/2127/5903663).
Older adults respond to their own stress and that experienced by staff, which can increase the risk of behavioral problems. Isolation and lack of stimulation may also lead to loneliness and depression. Each of these negative psychological outcomes has a significant impact on an individual’s immune system and the ability to fight infection.
An increasing number of patients recovering from COVID-19 are having lingering cognitive symptoms, including confusion and impaired executive functions, short-term memory issues, and learning difficulties. For those who had compromised cognitive-communication status before COVID-19, we need to be ready for ongoing exacerbation of symptoms.
New survey standards: Surveyors are advised to investigate any concerns as part of the focused infection control survey related to residents who have had a significant decline in condition. Emphasis is on decline with the resident’s condition, both physical and/or psychosocial.
Therapy Interventions must address the clinical changes in our patients from this pandemic.
Occupational Therapy Intervention/Strategies
● Measure the effects of cardiac function and respiration, including any increased oxygen and/or oxygen weaning with ADLs (respiratory rehab ADLs; OT COPD treatment protocol)
● Assess functional mobility — high fall risk
● Provide energy conservation and work simplification interventions
● Consider cognition, cognitive rehabilitation and occupational performance; and address cognitive impairments
● Address psychosocial (OT psychosocial interventions), mental health (AOTA OT’s role with mental health recovery), stress (HRV training), and coping-related PTSD or anxiety disorder post-COVID-19
● Community reintegration
Physical Therapy Intervention/Strategies
● Measure the effects of cardiac function and respiration, including any increased oxygen and/or oxygen weaning with physical performance (respiratory rehab physical exercise; PT COPD treatment protocol)
● Provide strength and mobility interventions — exercise prescription, fall risk, take longer to regain strength
o Note: For exercise prescription, go back to pulmonary rehab principles and exercise prescription for older adults and modify based on symptoms, vital signs and RPE
o Aerobic exercise, strength training, flexibility intervention
o It is critical that physical therapists are aware of the clinical implications of coagulopathy and the prevalence of venous thromboembolism (VTE) in patients diagnosed with and recovering from COVID-19 through the promotion of early mobility and physical activity
● Provide pain assessments and intervention
● Community reintegration as indicated
● Need for outpatient services
Speech-Language Pathology Intervention/Strategies
● Measure the effects of cardiac function and respiration, including any increased oxygen and/or oxygen weaning with communication and swallow (respiratory rehab breathing interventions and using resistive devices; SLP COPD treatment protocol)
● Assess effective communication as it relates to respiratory function
● Assess cognition (great opportunity to use comprehensive cognitive assessments), provide cognitive rehabilitation to address cognitive impairments
o Note: Studies are emerging that suggest some type of association between neurological symptoms and COVID-19. Symptoms like headache, stiff neck, and loss of taste and smell raise suspicion of central nervous system involvement.
● Assess swallow; airway protection and cough strength. Integrate resistive breathing devices for intervention.
● Assess for continued loss of taste and smell and how that impacts hydration and nutrition.
● Need for outpatient services.