
By Angela Ambrose, Contributing Writer
When you’re tired of doing the same old exercise routine, it’s easy to make excuses and skip workouts. Only 23 percent of adults meet the 2018 Physical Activity Guidelines set forth by the U.S Department of Health and Human Services. They strongly recommend:
- At least 150 to 300 minutes of moderate aerobic activity or 75-150 minutes of vigorous-intensity aerobic activity weekly
- Strength training of all major muscle groups two or more days per week
- Stretching and mindfulness activities such as yoga, tai chi or qigong
- Balance training to prevent falls
Adding more variety to your workouts can help you meet all of these important exercise guidelines each week. Not only will you find more enjoyment, but you will also be more likely to exercise longer and more consistently. Spice up your exercise routine by trying two or three of the following options:

- Find a workout buddy — After a long, exhausting day at work, a supportive friend can give you that little nudge you need to get off the couch and get moving. Because you will need to coordinate schedules with your partner, your exercise time will be plugged in to your calendar ahead of time, making it a higher priority. Doing an aerobic workout with a motivating partner has the potential to double your performance, according to a study by the Society of Behavioral Medicine.
 2. Try a group fitness class — Even if you’re exercising in a crowded gym, you can still feel lost and lonely if you’re climbing on the stair stepper in a dark corner or lifting weights by yourself. Most health clubs offer group fitness classes taught by nationally certified instructors. The group energy is contagious and can help you push through an especially challenging workout. From barbell and kickboxing to dance and yoga classes, you’ll find a wide range of options to build aerobic endurance, muscular strength and flexibility.
2. Try a group fitness class — Even if you’re exercising in a crowded gym, you can still feel lost and lonely if you’re climbing on the stair stepper in a dark corner or lifting weights by yourself. Most health clubs offer group fitness classes taught by nationally certified instructors. The group energy is contagious and can help you push through an especially challenging workout. From barbell and kickboxing to dance and yoga classes, you’ll find a wide range of options to build aerobic endurance, muscular strength and flexibility.
3. Get outdoors — Numerous studies show that exercising in the fresh air and sunshine elevates your mood, reduces tension and motivates you to work out longer and harder than exercising inside.
4. Join a team sport — When you were a kid, you never worried about counting steps or calories. You played catch, kickball or Frisbee simply because you enjoyed being with friends. Make exercise fun again by joining a recreational sports league such as softball, soccer or basketball or by taking up tennis or racquetball. Team sports are particularly beneficial because they create social connections and friendly competition. A study published in Mayo Clinic Proceedings shows that participating in partner and team sports is associated with longer lifespans than exercising alone because they combine the benefits of physical activity with stimulating social interaction.
catch, kickball or Frisbee simply because you enjoyed being with friends. Make exercise fun again by joining a recreational sports league such as softball, soccer or basketball or by taking up tennis or racquetball. Team sports are particularly beneficial because they create social connections and friendly competition. A study published in Mayo Clinic Proceedings shows that participating in partner and team sports is associated with longer lifespans than exercising alone because they combine the benefits of physical activity with stimulating social interaction.
5. Break it up into smaller portions —“I just don’t have time.” This is the No. 1 excuse for not (Insert Photo 5) working out regularly. Research shows that “exercise snacking” — engaging in small “snack-sized” portions of exercise throughout the day — can be an effective way to increase your physical activity, especially on days when your schedule is jam-packed. Taking the stairs instead of the elevator or walking to the corner restaurant for lunch all count as exercise. Too tired to hit the gym after work? Have an exercise “snack” of push-ups or sit-ups before dinner, instead of that plate of nachos.
6. Listen to upbeat, motivating music — When you listen to fast tempo music with a strong beat, your body naturally wants to follow the rhythm of the music. Energizing music can distract you from discomfort, increase your exercise intensity and increase your endurance as much as 15 percent, according to Costas Karageorghis, Ph.D., a leading expert on exercise and music research. Select music with the tempo or beats-per-minute (bpm) that correspond with the exercise you’re doing. The song’s bpm should mirror your target heart rate, according to the American Council on Exercise. (See chart for recommendations.)

7. Set SMART goals — Setting goals can help keep you motivated, but they work best when they’re clearly defined. For example, if your goal is to lose weight or build more upper body strength, use the SMART guidelines to make it specific, measurable, attainable, realistic and set within a defined time frame. Having trouble coming up with a motivating fitness goal? Sign up with a friend for a community walk, run or bike ride to support a charitable cause.
8. Track your progress — Download a free mobile fitness app to record your exercise progress, and wear a fitness tracking device such as a Fitbit or Apple watch to get instant feedback. Wearable technology may motivate you to increase your physical activity and serve as a daily reminder to keep moving.
9. Build up intensity slowly — If you’ve been sedentary for a while, gradually increase the exercise intensity and time you spend working out. Start with exercises like brisk walking, swimming or leisurely biking that pose minimal risk of injury. Enlist the help of a personal trainer, if you would like more guidance and a customized workout plan.
Variety adds more excitement and challenge to your exercise routine. If you’re having fun in your workouts, you’re more likely to log extra steps, burn more calories and go well beyond the U.S. Physical Activity recommendations, as well as your own personal fitness goals.
more likely to log extra steps, burn more calories and go well beyond the U.S. Physical Activity recommendations, as well as your own personal fitness goals.
WELL Challenge! Share your own stories about how you’re adding variety to your workout!
- If you have Instagram: From your Instagram account, share a picture and caption and remember to hashtag both #CAPLICOwell #CAPLICOnation
- Or, using your smartphone: Visit EnsignTherapy.com, click “WELL” at the top of the page, then click “Share your Story” from the top of the WELL Site. There you’ll find room to share a short story and upload a picture from your phone.
We look forward to seeing your inspiring stories as a collaborator to our WELL Project.
For more information on this topic or the latest health and fitness news, visit AngelaAmbrose.com or follow Angela on Facebook (@AmbroseHealthyLiving).


 In Utah, we are fortunate enough to have a Recreational Therapy Resource, Kami Archibald. Kami is a great partner with our therapy teams to find ways to further enhance the lives of our residents. Through this partnership, our facility Rec Therapists are becoming an integral part of the therapy teams. This all started when they asked to be educated about our “therapy world,” productivity and how Rec Therapy can support us.
In Utah, we are fortunate enough to have a Recreational Therapy Resource, Kami Archibald. Kami is a great partner with our therapy teams to find ways to further enhance the lives of our residents. Through this partnership, our facility Rec Therapists are becoming an integral part of the therapy teams. This all started when they asked to be educated about our “therapy world,” productivity and how Rec Therapy can support us.
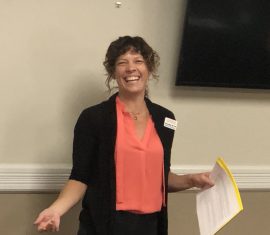
 An extensive interactive workshop with the Legend Oaks-New Braunfels team was conducted where the team had to design a room and bathroom with the appropriate colors, hues and tones in accordance with what we had learned about vision deficits and other physical and cognitive deficits present in dementia residents. Extensive education was provided about utilizing familiar designs with dementia care and the evidence surrounding this approach. “More familiar designs mean people with dementia are less likely to need help, that they make fewer mistakes and that they are more satisfied with the process than if the designs are unfamiliar.”
An extensive interactive workshop with the Legend Oaks-New Braunfels team was conducted where the team had to design a room and bathroom with the appropriate colors, hues and tones in accordance with what we had learned about vision deficits and other physical and cognitive deficits present in dementia residents. Extensive education was provided about utilizing familiar designs with dementia care and the evidence surrounding this approach. “More familiar designs mean people with dementia are less likely to need help, that they make fewer mistakes and that they are more satisfied with the process than if the designs are unfamiliar.” Meet Angela Ambrose. Angela is our latest partner contributing to our WELL Project and is a freelance writer with more than 30 years of writing experience. She is also an ACE-certified group fitness instructor and yoga teacher. When she’s not writing or teaching classes, Angela enjoys hiking, running and cooking up healthy Mediterranean-style meals for her family. Born and raised in Chicago, Angela moved to Phoenix 20 years ago and has settled comfortably into her home in the sunny Southwest. For the latest health and fitness news, visit AngelaAmbrose.com or follow Angela on Facebook (@AmbroseHealthyLiving).
Meet Angela Ambrose. Angela is our latest partner contributing to our WELL Project and is a freelance writer with more than 30 years of writing experience. She is also an ACE-certified group fitness instructor and yoga teacher. When she’s not writing or teaching classes, Angela enjoys hiking, running and cooking up healthy Mediterranean-style meals for her family. Born and raised in Chicago, Angela moved to Phoenix 20 years ago and has settled comfortably into her home in the sunny Southwest. For the latest health and fitness news, visit AngelaAmbrose.com or follow Angela on Facebook (@AmbroseHealthyLiving).
 Improve sleep. Daily exposure to sunlight naturally regulates circadian rhythms — your body’s internal clock — for a better night’s sleep. Regular exercise can further improve sleep quality by helping you get to sleep sooner and increasing deep sleep.
Improve sleep. Daily exposure to sunlight naturally regulates circadian rhythms — your body’s internal clock — for a better night’s sleep. Regular exercise can further improve sleep quality by helping you get to sleep sooner and increasing deep sleep. sunlight, it produces vitamin D3. This vitamin stimulates the absorption of calcium, which is essential in maintaining strong bones. Vitamin D also helps fight off infections. Deficiencies in vitamin D can increase the risk of developing heart disease, diabetes, autoimmune diseases and some cancers.
sunlight, it produces vitamin D3. This vitamin stimulates the absorption of calcium, which is essential in maintaining strong bones. Vitamin D also helps fight off infections. Deficiencies in vitamin D can increase the risk of developing heart disease, diabetes, autoimmune diseases and some cancers. Burn more calories. The constantly changing outdoor environment creates more challenges and stress on the body. Wind resistance can make you burn more calories, especially when you’re running or cycling into a headwind. Walking or jogging on an uneven, changing terrain also requires more muscle engagement than a flat, uniform surface. Your body must also work harder to regulate your internal temperature when exercising outdoors in hot or cold temperatures.
Burn more calories. The constantly changing outdoor environment creates more challenges and stress on the body. Wind resistance can make you burn more calories, especially when you’re running or cycling into a headwind. Walking or jogging on an uneven, changing terrain also requires more muscle engagement than a flat, uniform surface. Your body must also work harder to regulate your internal temperature when exercising outdoors in hot or cold temperatures.





 Deciding the Principle Medical Diagnosis, By Lori O’Hara, MA, CCC-SLP
Deciding the Principle Medical Diagnosis, By Lori O’Hara, MA, CCC-SLP