Partnering with Nursing: F-Tag 689
Submitted by Tamala Sammons, M.A. CCC-SLP, Sr. Therapy Resource
Federal Tags (F Tags) are the minimal Federal and State Standards of Care that are used to survey Skilled Nursing Facilities as a measure of performance. Rehab Services provides an important role in order to ensure compliance with these standards by having strong systems for IDT collaboration, patient identification, and providing skilled intervention programming.
“Assistance Device or Assistive Device” refers to any item (e.g., fixtures such as handrails, grab bars, and mechanical devices/equipment such as stand-alone or overhead transfer lifts, canes, wheelchairs, and walkers, etc.) that is used by, or in the care of a resident to promote, supplement, or enhance the resident’s function and/or safety.
- Are Safety Assessments part of therapy evaluations? Are they completed during different times of the day with various scenarios?
- How often does therapy engage in assessing assistance devices and providing staff education on proper use? How often does therapy assess to see if those devices are still the best option for each resident?
- Does therapy use a gait belt on patients anytime they require more than a supervision level of assistance?
- Is Therapy familiar with what’s on the care plan and helping to ensure it’s accurate for device usage?
- Is Therapy familiar with the CCA audit specific to this tag?
“Fall” refers to unintentionally coming to rest on the ground, floor, or other lower level, but not as a result of an overwhelming external force (e.g., a resident pushes another resident). An episode where a resident lost his/her balance and would have fallen, if not for another person or if he or she had not caught him/herself, is considered a fall. A fall without injury is still a fall. Unless there is evidence suggesting otherwise, when a resident is found on the floor, a fall is considered to have occurred.
- Do all disciplines get involved to determine who is a fall risk and what interventions to use?
- The evaluative phase for fall prevention shouldn’t end with one assessment. Patient behavior over time needs to be measured to determine the best interventions.
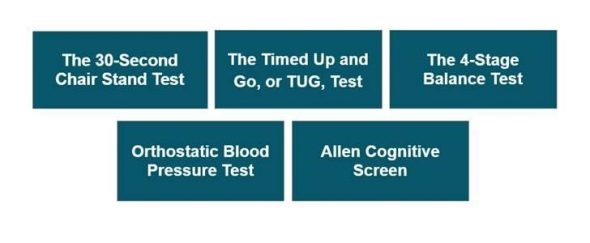
- Are we using various standardized tests that tell us who is at increased risk for falls such as:
- Do we assess gait velocity or just distance?
- Does therapy take time to ensure a new admit or a resident with a room change is oriented to their new environment? Is the environment set up in the best way for this patient’s success?
- Does Therapy use a gait belt on patients anytime they require more than a supervision level of assistance?
- Is Therapy familiar with the CCA audit specific to this tag?
- Does Therapy attend COC/Falls meetings?
Best Practice Ideas
- We have Therapy representation attending and contributing ideas for Incident and Fall meetings.
- We do ongoing therapy assessments for positioning, transfers, seating set up, etc. as fall prevention. NOTE: also ensure Care Plan is updated with the correct recommendations!
- We provide education to Nursing on how Therapy can help with both fall reduction and post-fall support. ALL disciplines! Be sure to cover how much SLP can do around cognition. Our SLPs work on fall reduction as much as PT!
- Therapy has increased communication to nursing in PCC in addition to various “paper forms” many facilities use.
- We do CNA huddles to ask about their concerns or recent changes with any residents.
- We complete a full battery of dx tests over more than one day to get a more comprehensive picture of how patients are performing.
- We participate in facility rounds/safety committee
- We participate in ongoing reviews of care plans for level of assist recommendations. We avoid ranges of assist (i.e., 1-2) and really dig into what each resident needs for that activity.
- We do an IDT post-fall meeting outside of a meeting room; we go to the resident and ask them to “re-enact” what happened. We assess environment and figure out any unmet needs of the resident at the time of the fall.
- Vital signs, vital signs, vital signs! We measure vital signs pre-, during, and post-treatment to assess for changes; we also complete orthostatic blood pressure testing on all residents and know who is at risk.
- Environment: We assess room setup, bathroom setup (i.e., does the current position of grab bars work for the residents in that room, toilet height, etc.).
- New admits and room changes: we assess the success of residents’ ability to function safely upon admission or after a room change (maybe they were closer to the bathroom and now they are not), as this is a new environment and it can be confusing to navigate, especially at night.
- Our OT has helped tremendously with our low vision population, adjusting the lighting in rooms and adding colored codes to remotes/call lights.
- We noticed a pattern of skilled patients falling within a day or two of admission. The Falls Team felt that this was due to the fact that there was no wheelchair available upon admission, as Nursing was waiting for Therapy to eval for transfers, etc. It led to patients attempting to transfer themselves because they did not have that visual reminder to wait for assistance. We attempted to solve this problem by having the rehab tech place a wheelchair in the patient rooms prior to admission so the reminder was there upon arrival. We noted a decline in subsequent falls around 18% month over month following this implementation.
- We noticed that quite a few falls were happening due to the patient’s need to toilet. The PTs jumped on board and decided to start a day shift toileting program whereby we scheduled time daily for the skilled patients who had fall risk factors. One therapist would have those patients scheduled for regular therapy and then follow up during the second half of their day to perform the toileting for the assigned patients for the day. They were successfully able to get those patients to the toilet twice throughout the four-hour shift, while also being able to bill time for functional activities as indicated. The two weeks we were able to run the program so far evidenced no falls on shift (and high patient satisfaction 😊). Our next step is to include all PTs and OTs on a rotating basis to perform toileting rounds on day shift and see how this impacts our falls.
- We communicate important updates and changes using the KARDEX for CNA/Nurse Easy Access.

