By Kai Williams, Therapy Resource, Keystone East, TX
There are many times that we run across clinicians that have such a passion for integrating new and innovative clinical ideas. Some move with hesitancy, unsure if their idea will really gain traction. We say to those that are hesitant, please Exercise your Passion for Learning! Malathy Venkatesh, PhD, CCC-SLP, originally joined our Mason Creek facility in Katy, Texas, in 2019. She recently relocated to our Tempe post-acute facility located in Arizona in late 2020. From the very first time I met Malathy, our conversations revolved around the underutilization of speech therapy services with a goal on how to increase awareness around clinical programming. Malathy has spent the last six months introducing LTC patients to the Montessori Method. Below you will find details about the Montessori approach to dementia from an SLP perspective, along with some ideas on how SLPs can use this approach in the LTC setting with examples of materials and goals.
Applying the Montessori Principles in the Management of Dementia: Speech Language
Pathologist’s Perspective
Malathy Venkatesh PhD CCC-SLP, Tempe Post-Acute, Tempe AZ
Speech Language Pathologists (SLPs) are constantly seeking approaches, materials and activities that place less demand on an impaired and progressively declining cognitive system such as the semantic and episodic memory, and more on engaging the relatively preserved procedural memory, to improve safety and functions in individuals with dementia. One approach that maximizes the preserved skills and abilities such as recognition of stimuli and reading is the Montessori approach for ageing and dementia. This approach, derived from the pedagogical approach to child education, has been developed and implemented successfully in adult day care centers and long-term care (LTC) settings.
One of the important principles of the Montessori approach is to encourage independence in individuals with dementia by engaging them in meaningful and purposeful activities in a prepared environment. The Montessori approach recommends that SLPs evaluate and manage individuals with dementia in their natural environment such as their rooms, dining room and activity room in addition to the clinical setting. The communication performance in a quiet therapy room may differ greatly from their communication abilities in a dining or activity room where they must adapt to the background noise and disproportionate visual stimulation. Two of the most common environmental barriers that affect the communication and interaction ability of individuals with dementia is light and contrast. The recommended environmental modifications for these barriers include incorporating bright but non-glare lighting in therapy spaces and reading spaces, minimizing unevenly lighted spaces, and preparing the environment where the figure contrasts from the background in such a way that it stands out, draws attention and is easy to locate.
The Montessori approach also relies heavily on “cueing,” using explicit visual cues in addition to verbal cues to facilitate initiation, maintenance and completion of an activity, and directions, signs around the facility, and memory books. Both texts and pictures are utilized while developing visual cues. Lighting and contrasts are important factors to be considered while displaying the visual cues. They should be displayed in a way that facilitates ease of recognition and reading and must fulfill the purpose that it intends to achieve, for example, locating rooms in the building.
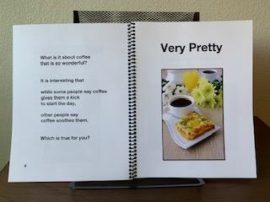
The Montessori approach taps on the relatively preserved ability of reading aloud by encouraging this skill as a pleasure activity utilizing dementia-friendly books. These books use large-print text with high-contrast pictures and illustrations. They are colorful and, more importantly, they are books designed for senior adults and adults with dementia. Reading books helps maintain language and reading skills, preserve pincer grasp when turning the pages, and maintain attention and focus. As shown in Figure 1, the environment is prepared ahead of the reading task by choosing a well-lit, quiet, distraction-free spot in the room. The book is mounted on a stand for easy reading and for page turning. Also notice that there are no shadows or glare on the book.
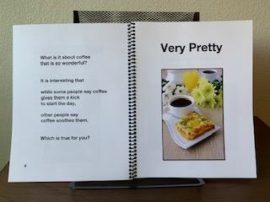
Figure 1: Dementia-friendly book (Courtesy of Susan Ostrowski, Reading2Connect at
www.Reading2Connect.com)
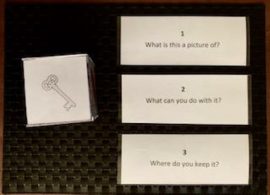
Another example applying the Montessori philosophy for a simple verbal expression task is utilizing a picture cube and wh-questions cue cards as illustrated in Figure 2. The purpose of this activity would be to facilitate word retrieval, improve comprehension of wh-questions, maintain language skills, maintain conversational skills, maintain attention and focus, and maintain reading skills. The level of complexity of the task can be modified based on the degree of impairment.
Figure 2: Verbal expression task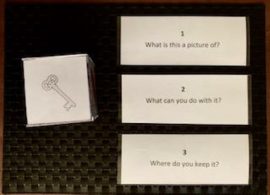
SLPs have a well-researched and successfully implemented approach that taps into the preserved abilities of individuals with dementia to address the impaired system, making their interactions more meaningful and improving their communication skills.
References:
Brush, J.A., (2020). Montessori for Elder and Dementia Care. Baltimore: Health Professions Press, Inc.
 When Sara Mohr, CFY at Sabino Canyon in Tucson, Arizona, was a SLP graduate student at the University of Arizona, the reality for those on modified diets became clear. Often a diagnosis of dysphagia brings confusion and worry. Getting modified diets right seems obvious, but actually can be quite hard. Options seemed few: mashed potatoes, blended meat and yogurt. She found few resources out there for patients in terms of appealing and tasty recipes with easy instructions for cooking and modifying.
When Sara Mohr, CFY at Sabino Canyon in Tucson, Arizona, was a SLP graduate student at the University of Arizona, the reality for those on modified diets became clear. Often a diagnosis of dysphagia brings confusion and worry. Getting modified diets right seems obvious, but actually can be quite hard. Options seemed few: mashed potatoes, blended meat and yogurt. She found few resources out there for patients in terms of appealing and tasty recipes with easy instructions for cooking and modifying.

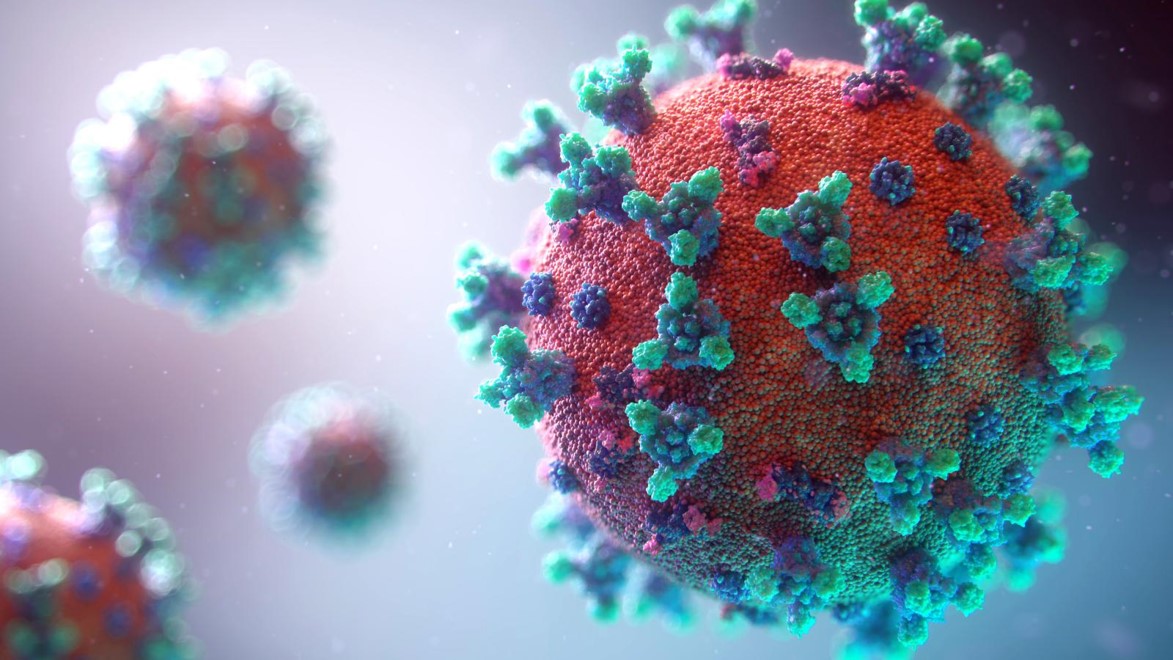
 COVID-19 is a respiratory viral disease with multi-organ involvement resulting in potentially temporary and episodic health challenges such as impaired lung function, physical deconditioning, cognitive impairments, impaired swallow and communication, and mental health disorders.
COVID-19 is a respiratory viral disease with multi-organ involvement resulting in potentially temporary and episodic health challenges such as impaired lung function, physical deconditioning, cognitive impairments, impaired swallow and communication, and mental health disorders.



 Caitlin Colteryahn is our lead occupational therapist here at The Healthcare Resort of Leawood and has been with us for four years. Caitlin graduated from Rockhurst University in 2014. She has been married for 10 years and has two boys. She loves spending time outdoors and traveling, especially with friends and family.
Caitlin Colteryahn is our lead occupational therapist here at The Healthcare Resort of Leawood and has been with us for four years. Caitlin graduated from Rockhurst University in 2014. She has been married for 10 years and has two boys. She loves spending time outdoors and traveling, especially with friends and family.

 All in the Family
All in the Family