By Brian del Poso, OTR/L, CHC, RAC-CT, Therapy Resource
 Through this difficult time, all of us are doing what we can to pitch in while at the facility, or remotely for those of us who can’t go to our facilities at the moment. With the stress of our jobs, schools being closed, scavenging for groceries, etc., it’s easy for us to forget about taking care of ourselves or make excuses for why we can’t take care of ourselves right now. We tell ourselves “I’m too tired from my crazy day”; “I have to find something for my kids to do”; “The gyms are all closed”; “If I don’t read all of Mary’s COVID-19 emails right at this moment, I won’t be prepared for tomorrow” (yes, people, it’s sarcasm) … well, STOP IT! Yup, a Bob Newhart reference, and if you don’t know what I’m talking about, check out this clip here. I promise, it’ll brighten your day! https://www.youtube.com/watch?v=Ow0lr63y4Mw
Through this difficult time, all of us are doing what we can to pitch in while at the facility, or remotely for those of us who can’t go to our facilities at the moment. With the stress of our jobs, schools being closed, scavenging for groceries, etc., it’s easy for us to forget about taking care of ourselves or make excuses for why we can’t take care of ourselves right now. We tell ourselves “I’m too tired from my crazy day”; “I have to find something for my kids to do”; “The gyms are all closed”; “If I don’t read all of Mary’s COVID-19 emails right at this moment, I won’t be prepared for tomorrow” (yes, people, it’s sarcasm) … well, STOP IT! Yup, a Bob Newhart reference, and if you don’t know what I’m talking about, check out this clip here. I promise, it’ll brighten your day! https://www.youtube.com/watch?v=Ow0lr63y4Mw
As therapists, we know that exercise is one of the best ways we can take care of ourselves, relieve stress and increase our happy hormones! Just STOP IT, and create 15 to 30 minutes for you and your well-being to do some exercise while at home. Here are samples of some simple, basic routines you can try (a quick Google search will give you an idea of how to do the exercise if you’re not sure):
No Weights … No Problem! Body-Weight Circuit It Is!
Perform each exercise in the circuit for 45 seconds at your own pace, with 15 seconds of rest between each exercise. You can increase progression simply by increasing the number of reps you can perform in the 45 seconds or by increasing your work time/decreasing your rest time.
Routine 1
– Squats (modify by how deep into the squat you go)
– Push-ups (modify by performing on your knees or against a wall/table)
– Walking lunges (modify by how deep you lunge)
– Plank
– Side lunges (modify by how deep you lunge)
– Mountain climbers (modify by how high you bring your knee toward your chest)
– Standing scapular retraction (3-5 second holds)
Routine 2
– Diamond push-ups (modify by performing on your knees or against a wall/table)
– Glute bridges
– Crunches
– Triceps dip on a chair (modify by bending your knees in your start position)
– Single leg Romanian deadlift
– Leg raises
– Door-frame rows (modify by body angle)
Feeling frisky? Perform two to three sets of the circuit with two to three minutes of rest between circuits, or grab some of those cans and bottles you bought from the grocery store and add some weight to the routine! (Pro Tip: You can use HeartMath with quick coherence in-between sets to concentrate and slow your breath, re-clarify and refocus for the next set … I know, MIND BLOWN)
But Wait, I Only Have 5 Minutes to Spare … Perfect, Tabatas Only Take 4 Minutes!
Tabata Training is a form of High Intensity Interval Training (HIIT) that requires 20 seconds of high intensity exercise (going all out!), followed by 10 seconds of rest, for eight rounds. This 4-minute method is a fat-burning, metabolism-boosting, sweat-drenching workout that is the equivalent to doing 20 minutes of normal cardio.
– High knees
– Burpees
– Jumping jacks
– Mountain climbers
– 20 seconds of all-out work, 10 seconds of rest between each exercise, repeat for a total of 8 rounds
Not into these types of exercises? Some other things you can try: March in place while you’re reading that book or watching your favorite show; take a few laps up and down your stairs if you’re in a multi-story home; chase that dog of yours around your home for a few minutes; you get the drift. Also, if you are already part of a local gym/fitness club, check in with them. Many companies are offering their members online home training options. The main thing is, don’t concentrate on what you can’t do anymore because of the restrictions in place, but focus on all of the things we can do, and just keep yourself active!
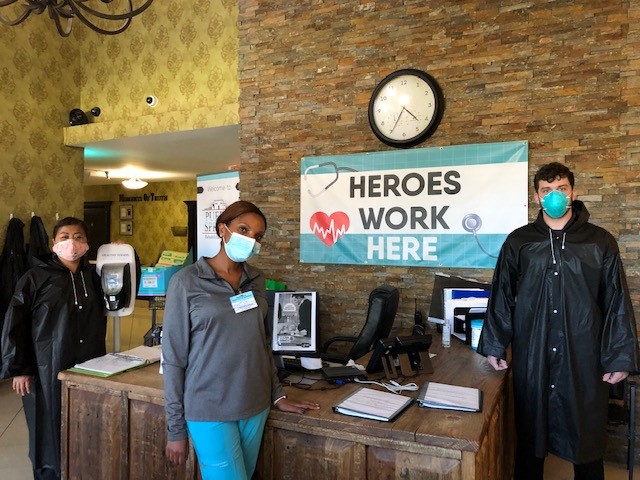
 The employees at City Creek Post-Acute in Salt Lake City, Utah, truly are superheroes. City Creek has partnered with the state to become a COVID-only building. As part of this partnership, City Creek was required to temporarily place their residents in sister facilities throughout the Salt Lake valley. This was a huge undertaking in and of itself and was the beginning of building something very special at City Creek.
The employees at City Creek Post-Acute in Salt Lake City, Utah, truly are superheroes. City Creek has partnered with the state to become a COVID-only building. As part of this partnership, City Creek was required to temporarily place their residents in sister facilities throughout the Salt Lake valley. This was a huge undertaking in and of itself and was the beginning of building something very special at City Creek.

 By Shelby Donahoo, M.S., OTR/L, Therapy Resource – Bandera
By Shelby Donahoo, M.S., OTR/L, Therapy Resource – Bandera
 The acquisition of St. Elizabeth Healthcare and Rehabilitation happened in May 2019. The transition was remarkably successful, but it did not come without challenges. Equipped with knowledge and guidance from our resources, we were ready for the speed bumps ahead — from changing guidelines of our managed care partners, new state and federal regulations to the Star Rating Data, onset of PDPM and many more. Our relentless, action-oriented and fearless yet compassionate leaders, Rand (Administrator) and Mady (Director of Nursing), knew that the only way to achieve these things is staying the course toward our true north — that of providing the best individualized care to all our residents while continuing to embody the CAPLICO values toward one another.
The acquisition of St. Elizabeth Healthcare and Rehabilitation happened in May 2019. The transition was remarkably successful, but it did not come without challenges. Equipped with knowledge and guidance from our resources, we were ready for the speed bumps ahead — from changing guidelines of our managed care partners, new state and federal regulations to the Star Rating Data, onset of PDPM and many more. Our relentless, action-oriented and fearless yet compassionate leaders, Rand (Administrator) and Mady (Director of Nursing), knew that the only way to achieve these things is staying the course toward our true north — that of providing the best individualized care to all our residents while continuing to embody the CAPLICO values toward one another.


 We invite anyone who is able and interested to join us with HeartMath at 8:30 a.m. Pacific daily during this time. Totally optional! You can join for one minute or join for longer. We would like to use the “Global Coherence App” that is available for free to download if you are able! Here are the instructions:
We invite anyone who is able and interested to join us with HeartMath at 8:30 a.m. Pacific daily during this time. Totally optional! You can join for one minute or join for longer. We would like to use the “Global Coherence App” that is available for free to download if you are able! Here are the instructions: