Did you know that there is a simple way to measure and reduce the stress response in our bodies? The variability in the heartbeat from beat to beat is called heart rate variability (HRV), and HRV is a powerful indicator of overall health. HRV essentially measures the stress response in our bodies, and through the use of biofeedback, we can actually train our stress response and improve our health! Dozens of our therapy programs across the country are using sophisticated biofeedback devices developed by our partners at HeartMath® in order to reduce personal stress, and to help our patients improve function and reduce anxiety. Here are a few examples of our success stories!
Did you know that there is a simple way to measure and reduce the stress response in our bodies? The variability in the heartbeat from beat to beat is called heart rate variability (HRV), and HRV is a powerful indicator of overall health. HRV essentially measures the stress response in our bodies, and through the use of biofeedback, we can actually train our stress response and improve our health! Dozens of our therapy programs across the country are using sophisticated biofeedback devices developed by our partners at HeartMath® in order to reduce personal stress, and to help our patients improve function and reduce anxiety. Here are a few examples of our success stories!
Angela Anderson at Gateway in Pocatello, Idaho, used the power of HeartMath technology to help a patient who was experiencing anxiety that would lead to cardiac arrhythmias resulting in multiple hospital readmission. Angela began biofeedback training using the HeartMath app and Bluetooth device, and the patient responded immediately with reduced anxiety. Angela set up the patient in her room with a portable device for her to use anytime she felt the anxiety and panic starting to occur. The results have been life-changing for the patient. She is now able to manage her anxiety and no longer is discharged to the hospital with panic attacks. The physicians and staff have been amazed!
Matt Zweig, Occupational Therapist at Park View Post-Acute Care, utilized HeartMath with a patient who came to the facility following a CABG. Even though the patient had just undergone extensive cardiac surgery, he had limited understanding of blood pressure and the anatomy and function of the heart. Matt used HRV training as an opportunity to educate the patient about the overall function of the heart. Matt hooked up the biofeedback device and instructed the patient on the techniques to regulate his autonomic nervous system. The patient was fascinated with the ability to see the results of the techniques through biofeedback and reported greatly reduced anxiety as a result of being able to regulate his heart.
Tyler Johnson, DOR at Northbrook, utilized the HeartMath biofeedback device with a patient with pneumonia, atrial fibrillation and anxiety. The patient was struggling to complete therapy sessions and quickly becoming short of breath (SOB). When the patient became SOB, he became more anxious and O2 saturations would quickly decrease. He was unable to complete functional mobility or ADLs due to SOB and O2 sat decline was also sent to the ER three times in a one-week period with these symptoms. HRV training was implemented with the use of the HeartMath emWave Pro to decrease anxiety, control rate of breathing and improve functional performance. The patient was able to maintain O2 saturations above 90 percent following HRV training and able to participate in training for functional transfers and ADLs with SBA.
Stephanie Winkler is a DOR at Wellington Rehab in Temple, Texas. Stephanie and her staff have multiple personal and patient success stories.
Mrs. T’s story:
Mrs. T had a variety of tests run as she was presenting with LE and UE weakness, but without any diagnosis to support the weakness. She was discharged from the hospital and was initially not making progress with therapy. We introduced the HRV training using HeartMath to see if we could help with focus and reduce her anxiety and depression. After only two sessions, she was able to focus better, participating in therapy and improving each day. She didn’t initially understand that she had underlying anxiety and fear, but with the use of HeartMath, she was able to control her anxiety and ambulate over 300 feet on even and uneven surfaces as well as shower and dress independently, and she was discharged home independently.
Mrs. S’s story:
Mrs. S came to us following a total knee replacement. She was exhibiting high anxiety and fear during her therapy. On the third day, we introduced the HRV training using HeartMath. Through the use of this program, she was able to begin to help with bed mobility and begin her rehabilitation with fewer episodes of yelling. She also was able to overcome her fear of standing and ambulate over 300 feet independently with the use of an assistive device, and she achieved excellent knee range of motion. The use of HRV biofeedback training allowed her to participate with therapy so that she quickly achieved independence with a short length of stay.
Mrs. B’s story:
Mrs. B came to us due to a hip fracture. She had a tremendous amount of fear and anxiety that was limiting her ability to participate in therapy. HRV training using HeartMath was introduced, and she was then able to fully participate in her therapy session, was following one-step commands, and was able to perform functional transfers and gait training with the assistance of therapy within the first week of HeartMath implementation.
Jon Anderson, Texas therapy resource, utilizes HRV and HeartMath both in trainings with therapy staff and also for his own health. One of the most profound changes that Jon has seen personally is his ability to sleep at night. He also has noticed an improved ability to focus and listen to others, reduced muscle tension, and overall reduced pain and fatigue after implementing the biofeedback techniques. Jon has also introduced the technology to his mother to help her with her anxiety and health challenges.


 The North Mountain Therapy Department specializes in Pulmonary Rehab, encouraging a multi-disciplinary approach to meet our respiratory patients’ goals of being decannulated, which typically is dependent upon the patient’s ability to return to a regular diet. In an effort to contribute to the greater independence of our patients, the Therapy Department created the SPOT (Speech Pathology Occupational Therapy), a holistic approach to a specialized dining experience to facilitate independence with safe swallow techniques and self-feeding.
The North Mountain Therapy Department specializes in Pulmonary Rehab, encouraging a multi-disciplinary approach to meet our respiratory patients’ goals of being decannulated, which typically is dependent upon the patient’s ability to return to a regular diet. In an effort to contribute to the greater independence of our patients, the Therapy Department created the SPOT (Speech Pathology Occupational Therapy), a holistic approach to a specialized dining experience to facilitate independence with safe swallow techniques and self-feeding.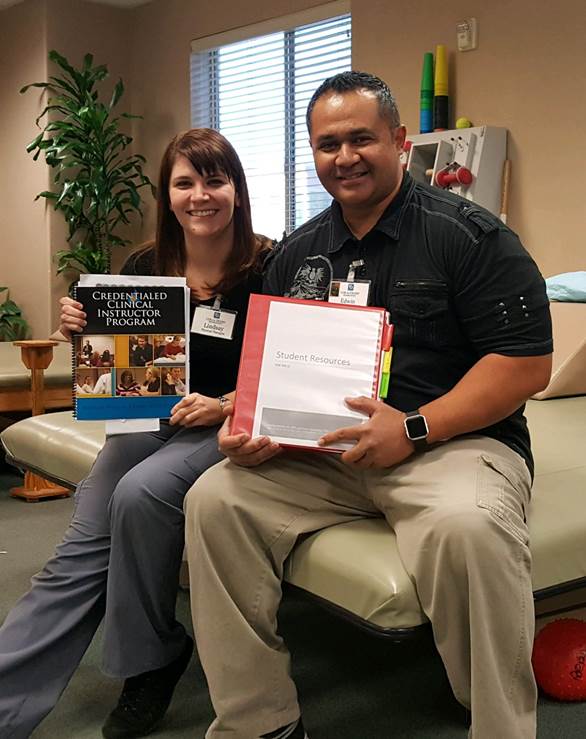
 What was initially simply a continuing education experience for two therapists has inspired a brand-new program here at Coral Desert Rehabilitation. Recently, a Coral Desert physical therapist, Lindsay Rankin, and a physical therapist assistant, Edwin Stevenson, attended a course to become credentialed clinical instructors. They both enjoy having students, so they were excited to go. After attending the course, they came back with a desire not only to improve their own abilities, but also to help revamp the student program at Coral Desert.
What was initially simply a continuing education experience for two therapists has inspired a brand-new program here at Coral Desert Rehabilitation. Recently, a Coral Desert physical therapist, Lindsay Rankin, and a physical therapist assistant, Edwin Stevenson, attended a course to become credentialed clinical instructors. They both enjoy having students, so they were excited to go. After attending the course, they came back with a desire not only to improve their own abilities, but also to help revamp the student program at Coral Desert.


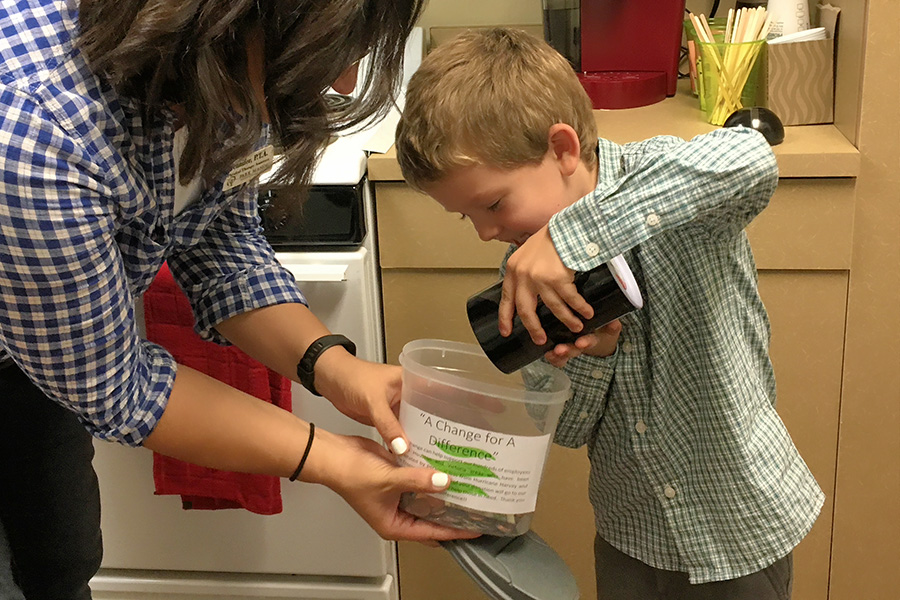 Park Manor raised over $3,500 for the EEF (Ensign Emergency Fund) to help those affected by Hurricane Harvey. The son of a PTA brought his piggy bank to pour into the EEF collection jar that was eventually filled with $240 in loose change!
Park Manor raised over $3,500 for the EEF (Ensign Emergency Fund) to help those affected by Hurricane Harvey. The son of a PTA brought his piggy bank to pour into the EEF collection jar that was eventually filled with $240 in loose change! Park Manor Therapy Team was represented in the Walk to End Alzheimer’s. Lots of bright colors and smiles to share!
Park Manor Therapy Team was represented in the Walk to End Alzheimer’s. Lots of bright colors and smiles to share! Preparing a meal with the Park Manor team at the Christian Aide Center. PT and ST and her family helped with the cooking and OT and his family helped with the serving along with other Park Manor staff.
Preparing a meal with the Park Manor team at the Christian Aide Center. PT and ST and her family helped with the cooking and OT and his family helped with the serving along with other Park Manor staff.


















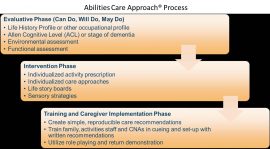
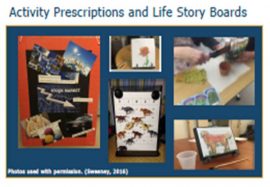 Clients with dementia living in skilled nursing facilities have occupational needs that are often unmet. Individualized care approaches and engagement in meaningful activities are effective non-pharmacologic approaches to dementia care. However, they are infrequently implemented in SNFs, and patients with dementia are often medicated with antipsychotic medications to manage behavioral symptoms related to dementia.
Clients with dementia living in skilled nursing facilities have occupational needs that are often unmet. Individualized care approaches and engagement in meaningful activities are effective non-pharmacologic approaches to dementia care. However, they are infrequently implemented in SNFs, and patients with dementia are often medicated with antipsychotic medications to manage behavioral symptoms related to dementia.