From Riverbend Post Acute Care, Kansas City, KS
By Madeana Galler, Therapy Resource
Riverbend nurses and therapists have united forces like never before. The two teams have joined forces to ensure the safety of all of their residents, and all the while gaining a deeper level of appreciation for one another through many Moments of Truth.
Jordanne Gerdes, COTA, and Amy Jacobs, PTA, have owned the shower schedule together with their partner CNAs. They also dried and styled the patients’ hair in preparation for Easter.
On April 9, 2020, TPM Justin Fricke’s church organized a prayer vigil for Riverbend, inviting the community via Facebook to come to the facility and pray over the facility, staff and residents. About 45 cars lined the parking lot, each person stayed in their car, a church member led the crowd in singing three hymns, followed by a short devotional on David and Goliath (overcoming COVID) and concluded with a prayer. There was an overwhelming feeling of support from the community, leaving many employees in tears of joy. Additionally, Justin’s wife’s work donated a truckload full of snacks and drinks to the facility.
Lisa Wainscott, OT, and her mother bought all the residents balloons. Lisa and Justin Smith, PT, personally passed out a balloon to each resident as a way of spreading love and gratitude.
Local restaurant, Mr. GoodcentsSubs, has donated grab-and-go style meals for the staff on a regular basis, and Plowboys BBQ donated meals for an entire week to the facility.
On April 13, 2020, Clinical Market Lead Maureen Purvis’ church family came to the facility and prayed over it.
Maureen Purvis, CML, Justin Fricke, TPM, Cory Schulte, ED and Jackie Brown, HR Resource, have been tirelessly and resolutely working together with the staff.
Facilities within the market sent handwritten posters with words of encouragement.




 By Jack Rolfe, PT, MNA, CHC, RAC-CT, Senior Compliance Partner for Utah
By Jack Rolfe, PT, MNA, CHC, RAC-CT, Senior Compliance Partner for Utah
 Hope Eaton (DON) and Sunny Chahal (DOR) at Eastview Healthcare in Houston, TX, have worked together for five years as a DOR/DON team. They both started working together while being new and have grown up by making mistakes together and finding solutions as a team. They call each other out on one another’s shortcomings and/or unproductive behaviors, but always make sure they genuinely apologize to one another when saying something inappropriate or something damaging to each other.
Hope Eaton (DON) and Sunny Chahal (DOR) at Eastview Healthcare in Houston, TX, have worked together for five years as a DOR/DON team. They both started working together while being new and have grown up by making mistakes together and finding solutions as a team. They call each other out on one another’s shortcomings and/or unproductive behaviors, but always make sure they genuinely apologize to one another when saying something inappropriate or something damaging to each other.
 The employees at City Creek Post-Acute in Salt Lake City, Utah, truly are superheroes. City Creek has partnered with the state to become a COVID-only building. As part of this partnership, City Creek was required to temporarily place their residents in sister facilities throughout the Salt Lake valley. This was a huge undertaking in and of itself and was the beginning of building something very special at City Creek.
The employees at City Creek Post-Acute in Salt Lake City, Utah, truly are superheroes. City Creek has partnered with the state to become a COVID-only building. As part of this partnership, City Creek was required to temporarily place their residents in sister facilities throughout the Salt Lake valley. This was a huge undertaking in and of itself and was the beginning of building something very special at City Creek.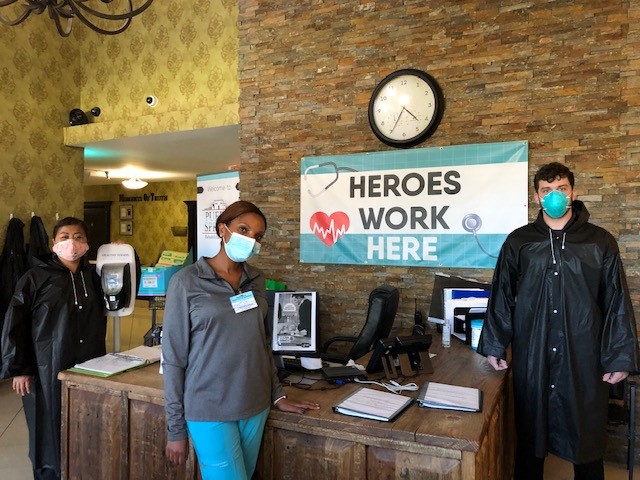
 By Shelby Donahoo, M.S., OTR/L, Therapy Resource – Bandera
By Shelby Donahoo, M.S., OTR/L, Therapy Resource – Bandera
 The acquisition of St. Elizabeth Healthcare and Rehabilitation happened in May 2019. The transition was remarkably successful, but it did not come without challenges. Equipped with knowledge and guidance from our resources, we were ready for the speed bumps ahead — from changing guidelines of our managed care partners, new state and federal regulations to the Star Rating Data, onset of PDPM and many more. Our relentless, action-oriented and fearless yet compassionate leaders, Rand (Administrator) and Mady (Director of Nursing), knew that the only way to achieve these things is staying the course toward our true north — that of providing the best individualized care to all our residents while continuing to embody the CAPLICO values toward one another.
The acquisition of St. Elizabeth Healthcare and Rehabilitation happened in May 2019. The transition was remarkably successful, but it did not come without challenges. Equipped with knowledge and guidance from our resources, we were ready for the speed bumps ahead — from changing guidelines of our managed care partners, new state and federal regulations to the Star Rating Data, onset of PDPM and many more. Our relentless, action-oriented and fearless yet compassionate leaders, Rand (Administrator) and Mady (Director of Nursing), knew that the only way to achieve these things is staying the course toward our true north — that of providing the best individualized care to all our residents while continuing to embody the CAPLICO values toward one another.
