Submitted by Cory Robertson, Therapy Resource, Pennant-Idaho
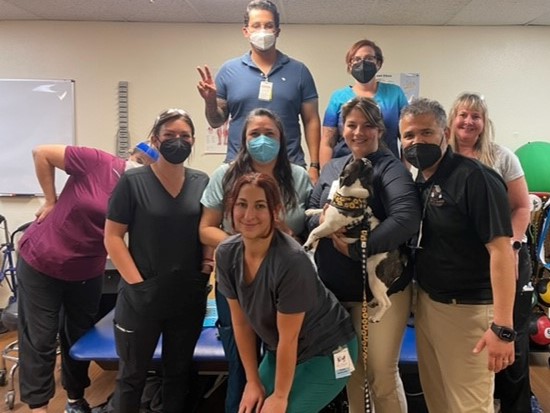
Discovery Rehab and Living in rural Salmon, Idaho, is a smaller facility in a mountainous rural setting that has been using contract therapy for years. Staffing is a large challenge and was seemingly a revolving door of therapy clinicians. Early last year, the contract company brought on a new leader. This leader demonstrated excellent drive and CAPLICO culture but without the same support from the contract therapy company that Ensign-affiliated facilities appreciate. Largely because of this leader, the facility ED Steve Lish, with cluster, market and resource assistance, decided to once again bring therapy in-house. Jolene Hugo, COTA/L, TPM, leads the Therapy team at Discovery Rehab and Living and exemplifies CAPLICO while managing the difficulties of a small rural therapy department like an all-star. Here are some of her reflections on the transition:
“May of this year marked our one-year anniversary for transitioning from contract therapy to in-house therapy at Discovery. When discussing the risks versus rewards of transitioning to in-house a year ago, I was intimidated. I felt nervous because I wanted to be able to prove that our therapy department could perform well. However, during and after the transition, I felt the weight of it all lifted by all of the support that being a part of Ensign Services has to offer our Therapy team and building. Being in-house really helped our Therapy department be part of a team and not just Therapy versus Them. I have a great resource and cluster partners that are readily available to work through difficult moments and the daily challenges. I have amazing opportunities to attend meetings that have helped me grow personally and professionally as a leader. Before being part of Discovery Care Center and our Ensign affiliates, , the challenges of the role really felt heavy, but now I have the resources to confront the challenges confidently.”