Say your patient had a hip replacement after a fall with a fracture. Coding rules say you code the fracture first, not the aftercare code. But that’s fine — as long as you check the box that says “Hip Replacement” in section J of the MDS, then the fracture code will automatically “bump” up into the Major Joint Replacement, right?
Wrong! The bump is not automatic. The fracture code that’s selected has to be eligible for re-categorization.
But how do I know? you are asking yourself.
Easy! Look at the map!
CMS has mapped every ICD-10 diagnosis to a category (or an RTP!), and the map will tell you if the code you’ve selected is eligible for re-categorization if it gets partnered with a surgery in the MDS. This is true for the bump into the Major Joint or Spinal Surgery as well as the Other Orthopedic Surgery category.
So where’s the map? The PDPM ICD-10 Map is available in the “Resource” tab in the “PDPM Ready 106 — Field Practice, Identifying the Primary Medical Condition” LMS training, or on the CMS.gov website (https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/SNFPPS/PDPM.html).
How do I read the map? When you find your diagnosis, look to see what the map says in the “Resident Had a Major Procedure during the Prior Inpatient Stay that Impacts the SNF Care Plan?” column. If it says “NA,” then checking the “hip replacement” box in the MDS won’t do a thing. But if it says, “May be Eligible for One of the Two Orthopedic Surgery Categories,” then checking the box will “bump” the code.
Let’s look at some examples from the map. Here are three femur fracture codes:
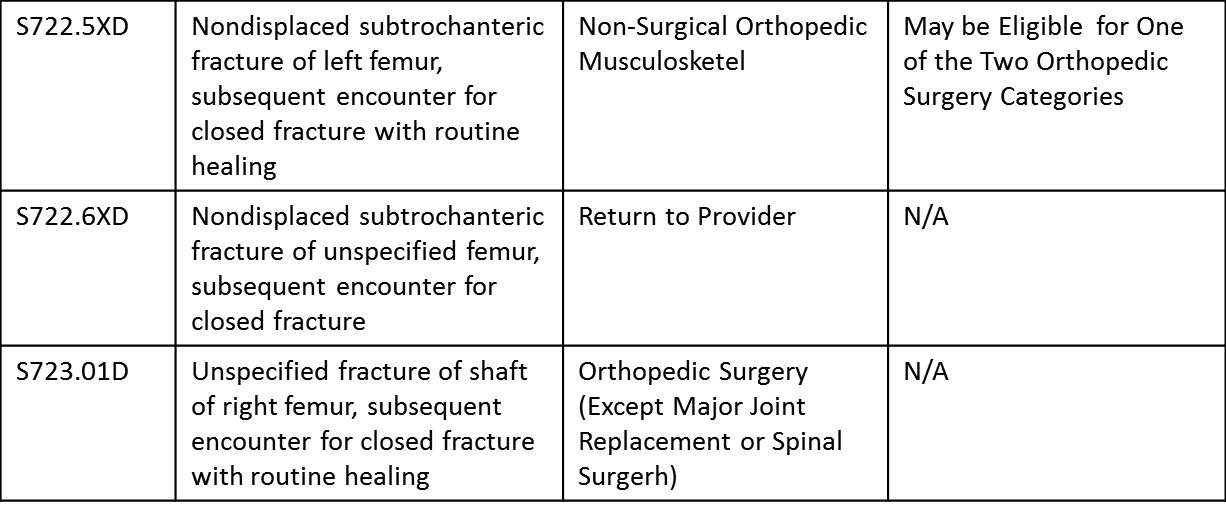
Look at the first code: S722.5XD describes a closed left femur fracture with routine healing. By itself, it would qualify only for the Non-Surgical Ortho category. But the box on the right says, “May be Eligible for One of the Two Orthopedic Surgery Categories.” So checking the “hip replacement” box in the MDS will bump this code into the category we should have — Major Joint Replacement.
The middle code (S722.6XD) describes a fracture of an unspecified femur. This is a Return to Provider (RTP) code. And with good reason — we can tell which femur was broken!
The bottom code (S723.01D) describes a closed fracture of the shaft of the right femur. This qualifies for an orthopedic surgery category, but look at the box on the far right — the one that tells you if the code is eligible for the bump. The box says, “NA.” This means if you used this code, even if you check the “Hip Replacement” box, the category wouldn’t change. This makes good clinical sense, since a fractured femur shaft isn’t when a hip replacement would be done. But what if that code got in there by accident and no one noticed? This is why close attention to codes is so important! The input of a therapist whose expertise includes the nature of fractures and joint replacements is a critical support to the team who is selecting the diagnoses.
So, the takeaway is that while CMS is happy to provide us with reimbursement commensurate with taking care of a major joint replacement or spinal surgery, we need to watch how we’re coding carefully so that we build the case in such a way that CMS can know that that’s what we’re doing.
By Lori O’Hara, MA, CCC-SLP, Therapy Resource – ADR/Appeals/Clinical Review