By Keystone Therapy
What started with a team’s desire to find a better way to treat LTC patients, morphed into a two-year ongoing journey, implementing the most recent evidence-based practice for their residents with dementia, leading them to the implementation of the Abilities Care Approach (ACA). ACA is a program that focuses on maximizing caregiver knowledge in dementia care. By doing so, it created a culture change within the facility that sparked an interest from dementia care to dementia design.
Dementia design is essentially a way to create the best environment for maximizing independence for persons living with dementia. In an Intelligent Risk, Legend Oaks-New Braunfels funded several team leaders to study dementia design at the University of Scotland, a world-renowned dementia design university where companies and facilities from all over the world have sought their accreditation and guidance in best practice for dementia design.
The training course began by presenting the increasing prevalence of dementia and the responsibility for those in the field to provide design and practice in accordance with what research has taught us about dementia. Three different models of how facilities operate when providing care to dementia residents were presented: Basic Needs, where only the basic needs of the resident are met; Social Model, where safety and security are the primary concerns; and a Bio-Psychosocial Model, which is an ambitious approach to care in dementia that takes into account individual needs and preferences, best design and care practice, along with needs and security. As they took an honest look into the approach utilized by their building, they were even more motivated to learn and implement the knowledge gained as they realized their building probably falls somewhere between a Basic Needs and a Safety/Security model.
Dementia design was introduced by an interior designer with extensive expertise in the field of dementia. The five primary dementia design principles taught during this session included: supporting individual needs, maximizing independence, reinforcing personal identity, making design orientating and understandable, and providing control and balance. Design features included: familiarity, reduction in stress and anxiety, clear visibility and multiple cues, and minimizing distractions. Design modifications and examples of other facilities were provided that achieve the five dementia design principles and design features. Color, hue and tone were explained in relation to dementia care and how to contrast design within the building to accommodate the deficits that present in dementia residents.
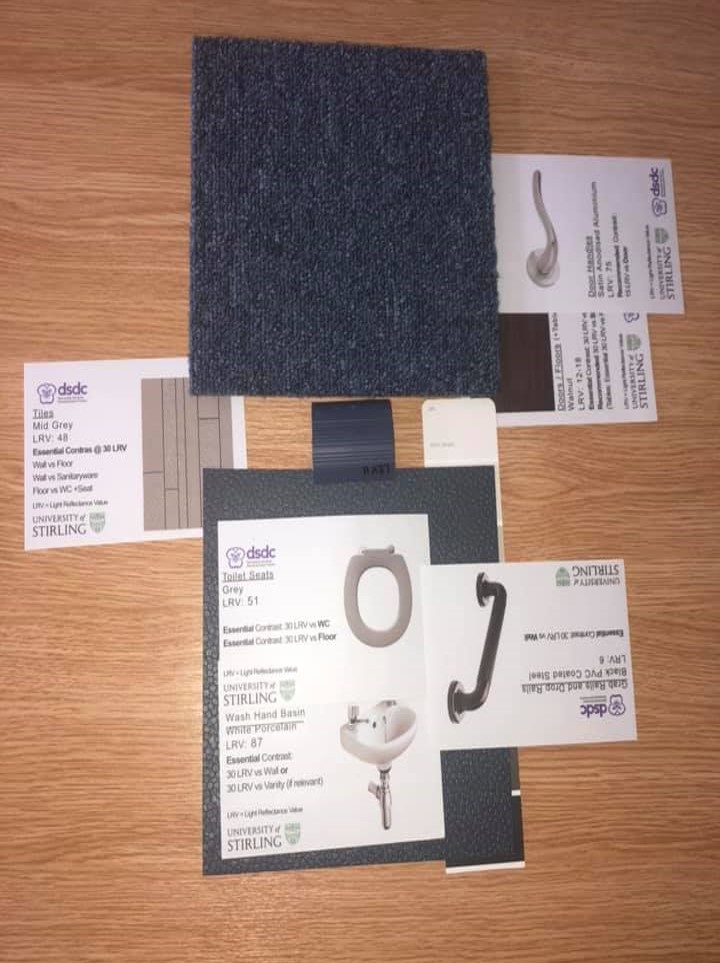
 An extensive interactive workshop with the Legend Oaks-New Braunfels team was conducted where the team had to design a room and bathroom with the appropriate colors, hues and tones in accordance with what we had learned about vision deficits and other physical and cognitive deficits present in dementia residents. Extensive education was provided about utilizing familiar designs with dementia care and the evidence surrounding this approach. “More familiar designs mean people with dementia are less likely to need help, that they make fewer mistakes and that they are more satisfied with the process than if the designs are unfamiliar.”
An extensive interactive workshop with the Legend Oaks-New Braunfels team was conducted where the team had to design a room and bathroom with the appropriate colors, hues and tones in accordance with what we had learned about vision deficits and other physical and cognitive deficits present in dementia residents. Extensive education was provided about utilizing familiar designs with dementia care and the evidence surrounding this approach. “More familiar designs mean people with dementia are less likely to need help, that they make fewer mistakes and that they are more satisfied with the process than if the designs are unfamiliar.”
The interior designer was then followed by an architect who specializes in dementia design. It was here the team learned extensive knowledge regarding appropriate lighting in the morning, afternoon and evening hours in accordance with what we know about dementia and brain function during these times. Appropriate lighting for dementia residents provides better performance throughout the day and good sleep routines, which is often difficult to accomplish in residents with dementia. Education regarding flooring consistency and knowledge on how to contrast floors with seating areas in accordance with vision deficits associated with dementia was explained in great detail to significantly decrease residents’ risk for falls and promote independence.
On the last day of training, the Legend Oaks team was able to tour educational rooms designed in accordance with the principles taught in class. These rooms included: bedrooms, bathrooms, hallways, stairs and a hospital. The team was required to inspect each room and “tag” any errors found in accordance with knowledge gained during the courses.
Legend Oaks-New Braunfels is hoping to seek a partnership with the University of Stirling as they begin their next grant that will focus on dementia design and the knowledge gained during their training courses. The team is already laser-focused on next steps and is diligently working to pave the way for dementia design in the United States, as well as provide cutting-edge research and care for residents with dementia.

 Meet Andy! Satyanand Miyyapuram, better known as “Andy,” is an amazing PT at our Golden Acres building in Dallas.
Meet Andy! Satyanand Miyyapuram, better known as “Andy,” is an amazing PT at our Golden Acres building in Dallas. Meet Angela Ambrose. Angela is our latest partner contributing to our WELL Project and is a freelance writer with more than 30 years of writing experience. She is also an ACE-certified group fitness instructor and yoga teacher. When she’s not writing or teaching classes, Angela enjoys hiking, running and cooking up healthy Mediterranean-style meals for her family. Born and raised in Chicago, Angela moved to Phoenix 20 years ago and has settled comfortably into her home in the sunny Southwest. For the latest health and fitness news, visit AngelaAmbrose.com or follow Angela on Facebook (@AmbroseHealthyLiving).
Meet Angela Ambrose. Angela is our latest partner contributing to our WELL Project and is a freelance writer with more than 30 years of writing experience. She is also an ACE-certified group fitness instructor and yoga teacher. When she’s not writing or teaching classes, Angela enjoys hiking, running and cooking up healthy Mediterranean-style meals for her family. Born and raised in Chicago, Angela moved to Phoenix 20 years ago and has settled comfortably into her home in the sunny Southwest. For the latest health and fitness news, visit AngelaAmbrose.com or follow Angela on Facebook (@AmbroseHealthyLiving).
 Improve sleep. Daily exposure to sunlight naturally regulates circadian rhythms — your body’s internal clock — for a better night’s sleep. Regular exercise can further improve sleep quality by helping you get to sleep sooner and increasing deep sleep.
Improve sleep. Daily exposure to sunlight naturally regulates circadian rhythms — your body’s internal clock — for a better night’s sleep. Regular exercise can further improve sleep quality by helping you get to sleep sooner and increasing deep sleep. sunlight, it produces vitamin D3. This vitamin stimulates the absorption of calcium, which is essential in maintaining strong bones. Vitamin D also helps fight off infections. Deficiencies in vitamin D can increase the risk of developing heart disease, diabetes, autoimmune diseases and some cancers.
sunlight, it produces vitamin D3. This vitamin stimulates the absorption of calcium, which is essential in maintaining strong bones. Vitamin D also helps fight off infections. Deficiencies in vitamin D can increase the risk of developing heart disease, diabetes, autoimmune diseases and some cancers. Burn more calories. The constantly changing outdoor environment creates more challenges and stress on the body. Wind resistance can make you burn more calories, especially when you’re running or cycling into a headwind. Walking or jogging on an uneven, changing terrain also requires more muscle engagement than a flat, uniform surface. Your body must also work harder to regulate your internal temperature when exercising outdoors in hot or cold temperatures.
Burn more calories. The constantly changing outdoor environment creates more challenges and stress on the body. Wind resistance can make you burn more calories, especially when you’re running or cycling into a headwind. Walking or jogging on an uneven, changing terrain also requires more muscle engagement than a flat, uniform surface. Your body must also work harder to regulate your internal temperature when exercising outdoors in hot or cold temperatures.
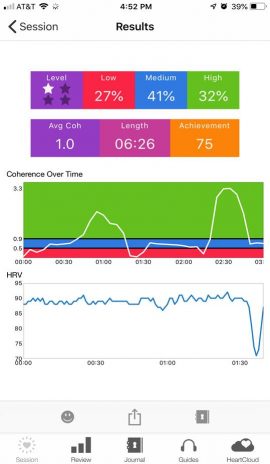 cer. One of her goals is to get stronger to be able to tolerate a chemotherapy treatment regimen. The team’s new COTA, Jay, decided to try HRV training to reduce pain and increase function. During the first session, the patient was able to briefly get into what is called neurological coherence, as indicated on the biofeedback device as the green zone. However, the pain quickly brought her out of coherence. Jay decided to try another technique. He asked her about one of her favorite places to be, and she told him it was Hawaii. Jay pulled up some Hawaiian music and talked her through the coherence steps, and she was very soon able to sustain coherence. What is really amazing is that she had been refusing physical therapy treatments due to pain, but after her session with Jay, she was able to participate in a full PT treatment, with a smile on her face. The biofeedback readings below show the spike in coherence when her favorite music and memories were introduced.
cer. One of her goals is to get stronger to be able to tolerate a chemotherapy treatment regimen. The team’s new COTA, Jay, decided to try HRV training to reduce pain and increase function. During the first session, the patient was able to briefly get into what is called neurological coherence, as indicated on the biofeedback device as the green zone. However, the pain quickly brought her out of coherence. Jay decided to try another technique. He asked her about one of her favorite places to be, and she told him it was Hawaii. Jay pulled up some Hawaiian music and talked her through the coherence steps, and she was very soon able to sustain coherence. What is really amazing is that she had been refusing physical therapy treatments due to pain, but after her session with Jay, she was able to participate in a full PT treatment, with a smile on her face. The biofeedback readings below show the spike in coherence when her favorite music and memories were introduced.
 It’s easy to get caught up in the day-to-day routine in this line of work. You have new programs you want to start, financial markers you strive to hit, and all of this trickles down to your team. However, every so often, you are reminded of why you chose this profession. It’s the people, their stories, their lives, and all they share.
It’s easy to get caught up in the day-to-day routine in this line of work. You have new programs you want to start, financial markers you strive to hit, and all of this trickles down to your team. However, every so often, you are reminded of why you chose this profession. It’s the people, their stories, their lives, and all they share.
 Kiran’s favorite recreation is playing with her two small children in her favorite place — her home. “I am a homebody and not very fond of traveling and adventuring. I love to stay home and spend quality time with my family and kids — this is the most beautiful place for me,” Kiran says.
Kiran’s favorite recreation is playing with her two small children in her favorite place — her home. “I am a homebody and not very fond of traveling and adventuring. I love to stay home and spend quality time with my family and kids — this is the most beautiful place for me,” Kiran says.
 Gordon Murray, Rehab Tech, has worked at North Mountain Medical and Rehab Center for over 14 years. Gordon has built many friendships with residents over the years due to his calm, gentle approach with residents. Gordon has a gift for motivating therapy patients, builds special bonds with them and has been referred to as “The Patient Whisperer” by his peers!
Gordon Murray, Rehab Tech, has worked at North Mountain Medical and Rehab Center for over 14 years. Gordon has built many friendships with residents over the years due to his calm, gentle approach with residents. Gordon has a gift for motivating therapy patients, builds special bonds with them and has been referred to as “The Patient Whisperer” by his peers!