 You have values and you OWN the responsibility for being ACCOUNTABLE to your team for knowing and following the rules governing your practice. You have a PASSION FOR LEARNING. And, with the moving target that healthcare regulation has become, your VALUES are the key to success. Your resource team is committed to keeping you abreast of some of the changes we are directly experiencing in our industry today, as well as the plans for implementation of other changes to come in the very near future.
You have values and you OWN the responsibility for being ACCOUNTABLE to your team for knowing and following the rules governing your practice. You have a PASSION FOR LEARNING. And, with the moving target that healthcare regulation has become, your VALUES are the key to success. Your resource team is committed to keeping you abreast of some of the changes we are directly experiencing in our industry today, as well as the plans for implementation of other changes to come in the very near future.
As you know, on February 22, 2012, President Obama signed into law the Middle Class Tax Relief and Jobs Creation Act of 2012 (HR 3630, Section 3005), which carried with it several implications for therapy service delivery under the Medicare Program. Some of the more relevant items specific to HR 3630 included:
- It prevented the expected 27.4% cut to the Medicare Physician payment rates (Part B Fee Screen), which were included in the Affordable Care Act. Instead, the signing of HR 3630 kept the rates frozen at their current levels through December 31, 2012.
- The Therapy Cap Exceptions Process was extended through December 31, 2012.
- All Claims above the Cap of $1880 are to be rejected without the KX modifier AND are subject to post-payment Manual Medical Review (MMR)
- A Pre-Authorization Process, which includes MMR, is now required for claims above a threshold of $3700 for PT and SLP Services Combined and a separate threshold of $3700 for OT Services.
- The spending caps and thresholds were extended to Hospital Outpatient Departments and Outpatient Rehab Agencies.
- Beginning January 1, 2013, CMS is required to collect data to assist in reforming the payment system for therapy services on patient function.
- In May 2013, the General Accounting Office (GAO) is required to submit a report to congress on the financial outcome of the MMR Process.
- In June 2013, MedPAC is required to submit a report on the Outpatient Therapy Payment System.
Your therapy resource team is actively engaged in gathering the most pertinent and up-to-date information from CMS and the Medicare Administrative Contractors (MAC’s) regarding the Manual Medical Review process. We are committed to providing clear and consistent communication and resources as this information becomes available. For example, we are actively engaged in working with partners of the National Association for the Support of Long Term Care (NASL) to identify strategies for improving the processes. We also have an avenue for sharing our concerns regarding the inconsistencies within the MMR process.
Our partnership with RehabOptima has provided us with technology to help us more effectively manage the aggressive changes to processes in billing and tracking authorization. The most recent version of RehabOptima (4.13), released on October 1, 2012, includes several new components for managing the Medicare Part B threshold, MMR process and Cap management. If you haven’t noticed, please take time, to read the release items located under “Release Notes” through the “Help” button on the tool bar.
We are watching closely for the new Final Rule on the Claims Based Data Collection Strategy expected to be released by CMS on November 1, 2012. This new rule is designed to assist in reforming payment for outpatient therapy services and is intended to provide for data collection on patients receiving outpatient therapy services. The initial data collection system suggested is a 12-point scale that is considered to be untested, unreliable and has not been validated. However, work groups comprised of members from APTA, AOTA, ASHA, NASL and others have been presenting alternatives to CMS. While this new rule is scheduled to go into effect on January 1, 2013, some are suggesting that it may need to be delayed or rolled out in phases, due to the concerns surrounding the tool that was initially proposed.
Your therapy resource team will continue to stay on top of these regulatory changes which impact our service delivery. We are involved in CMS Feedback and workgroups. We are continuing our partnership with RehabOptima, and we are working to remodel our Therapy Portal Resources and Training Programs to provide a more systematic approach to giving you the tools you need to continue your quest toward inspiring true greatness by living your values each and every day. You’ve got IT!
by Deb Bielek, Therapy Resource








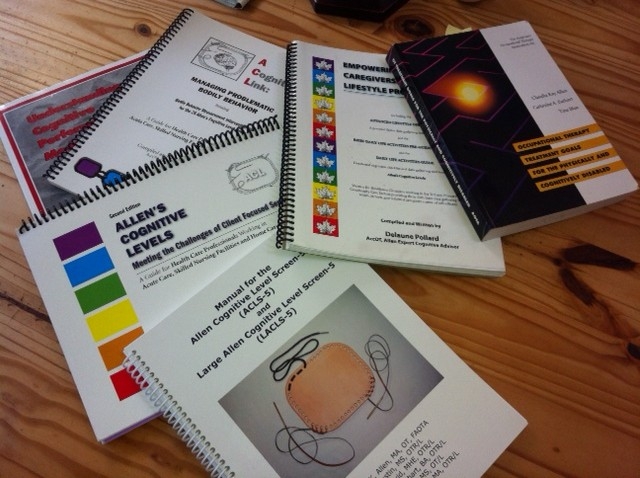
 In the United States, dementia is the most common diagnosis for nursing home residents, and the prevalence of dementia may be as high as 74 percent in nursing homes (Magaziner et al., 2000). You may have seen the statistic that 5.4 million Americans have Alzheimer’s dementia (Alzheimer’s Association, 2011), but did you know that another 5.4 million Americans over the age of 70 have cognitive impairment without dementia (Plassman et al., 2008)?
In the United States, dementia is the most common diagnosis for nursing home residents, and the prevalence of dementia may be as high as 74 percent in nursing homes (Magaziner et al., 2000). You may have seen the statistic that 5.4 million Americans have Alzheimer’s dementia (Alzheimer’s Association, 2011), but did you know that another 5.4 million Americans over the age of 70 have cognitive impairment without dementia (Plassman et al., 2008)?
