 Miriam Janove, PT, is an August 2019 graduate of the University of Puget Sound, Washington.
Miriam Janove, PT, is an August 2019 graduate of the University of Puget Sound, Washington.
Read her winning Essay below:
Jack (name changed for confidentiality) was admitted to inpatient rehab with a left pontine stroke, presenting with dense right hemiparesis and neglect. Three weeks later, he discharged from inpatient rehab with all his goals met, including transferring and walking with no physical assistance and hemi-propelling a wheelchair up and down ramps. The glow and satisfaction of a physical therapist is palpable when discharging a patient who has met all their goals and returned to all their prior activities. So often, however, we discharge patients who have plateaued below what we deemed as within their capacity at initial evaluation. There may be some structural differences between the bodies of the patients in these scenarios, but more concerning are the disparities in their attitudes and perspectives required for healing, such as an internal locus of control, therapeutic alliance and body awareness. Though physical therapy treatment should be based on therapeutic exercise, including strength, endurance, flexibility and coordination, to most effectively treat our patients, we must empower them to believe in the gains made through their own hard work and to engage fully in therapy.
We spend much of our Doctor of Physical Therapy (DPT) program learning about the structures and functions of the body in order to use evidence-based practice to treat our patients. Recently, we have shifted focus towards examining the impact of illness by discussing the patients’ participation goals using the International Classification of Functioning, Disability and Health (ICF) model. No longer is it appropriate to treat impairments in patients without accounting for the fact that we are working with human beings who have rich and demanding lives. I envision using my current and future studies to support the integration of patients’ humanity into medical treatment.
In Jack’s case, it was essential to account for the privacy that he and his wife value, as well as his wife’s inability to assist physically due to her own medical conditions. Due to their private natures, they were unwilling to ask neighbors or extended family for support. Additionally, he was obese and had a very sedentary lifestyle prior to his stroke, which left his intact side too weak to compensate for his hemiparesis.
Putting patients’ concerns and connections first lays a foundation for success in therapy, but there are several other relevant mental components to fruitful therapy. Locus of control is a concept that elucidates the perception of what impacts the outcomes in one’s life. Someone with an external locus of control believes that they have no direct influence over their own life. This person is likely to have significant difficulty with motivation to engage in therapeutic exercise because their perception is that their own actions will not impact their outcomes. However, someone with an internal locus of control believes that their actions directly influence their life.
Jack arrived at inpatient rehab with an external locus of control. He did not take responsibility for his own healing and did not prioritize exercise outside of therapy time. He had a defeated attitude and was resigned to his new immobility. As we know, therapeutic exercise during physical therapy sessions is insufficient for substantial progress, but despite reminders, he spent his evenings resting instead of exercising.
Though every individual has an innate tendency towards either an internal or external locus of control based on their personality, medical professionals can cultivate an increased internal locus of control in their patients through motivational interviewing and encouragement. Communicating to a patient that measurable improvements in strength, flexibility, endurance or coordination are due to the effort they put into their home exercise program helps foster a greater sense of internal locus of control. This internal locus of control is an asset that serves patients beyond one episode of care as they take ownership of their own health and healing overall.
Gentle encouragement for Jack to participate in the variety of therapeutic opportunities offered on inpatient rehab initially went nowhere. His external locus of control was apparent and he made excuses. As he slowly began to recognize strength gains within his own body, drawing the connection between those improvements and his effort helped him see the control he had over his own healing. After planting the seed, this internal locus of control took on a life of its own, growing exponentially each day as his functional mobility improved, first with independence in bed mobility, then transfers, and finally gait.
Motivational interviewing is a technique I used to build Jack’s internal locus of control. This technique allows medical professionals, including physical therapists, to help guide lifestyle changes by allowing patients to come to conclusions for themselves about their own priorities. By using open-ended questions, active listening and reflective statements, we can draw out our patients’ own reasons to make the changes we have already assessed to be beneficial. Many people resist demands and suggestions from medical professionals, but with motivational interviewing, the patient realizes through their own words that there is dissonance between their goals and their actions. People are more likely to commit to change if they are the ones to come up with the idea.
In talking with Jack, we discovered that his dogs were one of the most important things in his life. When thinking about caring for his dogs, he could see the real-life implications of working to increase his independence in mobility. He realized that his wife would become solely responsible for dog care if he didn’t work hard and improve his function. He wants to be a contributing member of society, and to Jack that means being a contributing member of his household.
Another elusive contributor to good outcomes in physical therapy is therapeutic alliance. This is a quality of the relationship built between therapist and patient, including trust, communication and collaboration. In a systematic review, Hall, et al. conclude that positive therapeutic alliance correlates with physical therapy outcomes including decreased pain, improved function, increased home exercise program compliance and increased satisfaction.1 Soft skills, such as listening and motivational interviewing are integral to building therapeutic alliance with patients who have clear benefits.
People can tell when someone is genuinely excited to spend time with them. It was enjoyable to work with Jack because he was pleasant, though he was not always cooperative. Motivational interviewing not only helps us understand the driving factors in our patients’ lives; it also helps us see their humanity. This connection builds compassion which supports therapeutic alliance by boosting each therapist to show up with true caring for each and every patient.
By bringing locus of control, motivational interviewing and therapeutic alliance to the forefront of physical therapy treatment, we will improve the care provided to one of the most challenging populations to treat, people with chronic pain. As the United States population ages, chronic pain has become an epidemic, which is beginning to get the attention it deserves. Chronic pain patients are a difficult population to treat because there is no protocol or quick fix. This group is also one of the biggest beneficiaries of cognitively based therapeutic interventions as a major part of their treatment program. We know that thoughts and breathing can impact patients’ blood pressures and heart rates, so it follows that thoughts and breathing also impact patients’ experience of pain.
Interdisciplinary collaboration is an important aspect of treating patients with chronic pain, since cognitive behavioral therapy is outside of our scope of practice as physical therapists. As with any other interdisciplinary work, physical therapists can support the goals and strategies of other therapists. We can use cognitively based techniques, such as mindfulness and visualization, learned from these other professionals, to enhance their practice and our own. Due to a flaccid arm and shoulder subluxation, Jack had shoulder pain. With diaphragmatic breathing and progressive muscle relaxation, his shoulder pain decreased. Another benefit of these activities is that they can be prescribed for times when a patient is too tired to do physical exercise.
As physical therapists, decreasing pain is a daily goal with many patients. Body awareness contributes to increasing patients’ locus of control and decreasing pain. Body awareness can be cultivated with widely accepted therapeutic interventions, such as diaphragmatic breathing and attention to exercise form, which is a form of mindfulness. Though some would argue that mindfulness training and meditation are outside of the physical therapy scope of practice, researchers have found that with proper training, these are effective and important tools within a physical therapy context.2, 3
People throughout the United States are frequently disgusted by the medical system. As physical therapists, we are players in their medical care with an opportunity to build connection and provide patients with caring and compassionate medical treatment. Building faith and trust between patients and the medical establishment improves patient outcomes, but more importantly improves people’s lives. By continuing to educate myself and others about the psychosocial and cognitive components of successful therapeutic relationships, I will help build a physical therapy community which treats the whole person instead of simply treating their body.
References
- Hall AM, Ferreira PH, Maher CG, Latimer J, Ferreira ML. The Influence of the Therapist-Patient Relationship on Treatment Outcome in Physical Rehabilitation: A Systematic Review. Physical Therapy. 2010;90(8):1099-1110. doi:10.2522/ptj.20090245.
- Pike AJ. Body-mindfulness in physiotherapy for the management of long-term chronic pain. Physical Therapy Reviews. 2008;13(1):45-56,doi:10.1179/174328808X251957
- Rundell SD, Davenport TE. Patient Education Based on Principles of Cognitive Behavioral Therapy for a Patient With Persistent Low Back Pain: A Case Report. Journal of Orthopaedic & Sports Physical Therapy. 2010;40(8):494-501

 Meet Andy! Satyanand Miyyapuram, better known as “Andy,” is an amazing PT at our Golden Acres building in Dallas.
Meet Andy! Satyanand Miyyapuram, better known as “Andy,” is an amazing PT at our Golden Acres building in Dallas. Meet Angela Ambrose. Angela is our latest partner contributing to our WELL Project and is a freelance writer with more than 30 years of writing experience. She is also an ACE-certified group fitness instructor and yoga teacher. When she’s not writing or teaching classes, Angela enjoys hiking, running and cooking up healthy Mediterranean-style meals for her family. Born and raised in Chicago, Angela moved to Phoenix 20 years ago and has settled comfortably into her home in the sunny Southwest. For the latest health and fitness news, visit AngelaAmbrose.com or follow Angela on Facebook (@AmbroseHealthyLiving).
Meet Angela Ambrose. Angela is our latest partner contributing to our WELL Project and is a freelance writer with more than 30 years of writing experience. She is also an ACE-certified group fitness instructor and yoga teacher. When she’s not writing or teaching classes, Angela enjoys hiking, running and cooking up healthy Mediterranean-style meals for her family. Born and raised in Chicago, Angela moved to Phoenix 20 years ago and has settled comfortably into her home in the sunny Southwest. For the latest health and fitness news, visit AngelaAmbrose.com or follow Angela on Facebook (@AmbroseHealthyLiving).
 Improve sleep. Daily exposure to sunlight naturally regulates circadian rhythms — your body’s internal clock — for a better night’s sleep. Regular exercise can further improve sleep quality by helping you get to sleep sooner and increasing deep sleep.
Improve sleep. Daily exposure to sunlight naturally regulates circadian rhythms — your body’s internal clock — for a better night’s sleep. Regular exercise can further improve sleep quality by helping you get to sleep sooner and increasing deep sleep. sunlight, it produces vitamin D3. This vitamin stimulates the absorption of calcium, which is essential in maintaining strong bones. Vitamin D also helps fight off infections. Deficiencies in vitamin D can increase the risk of developing heart disease, diabetes, autoimmune diseases and some cancers.
sunlight, it produces vitamin D3. This vitamin stimulates the absorption of calcium, which is essential in maintaining strong bones. Vitamin D also helps fight off infections. Deficiencies in vitamin D can increase the risk of developing heart disease, diabetes, autoimmune diseases and some cancers. Burn more calories. The constantly changing outdoor environment creates more challenges and stress on the body. Wind resistance can make you burn more calories, especially when you’re running or cycling into a headwind. Walking or jogging on an uneven, changing terrain also requires more muscle engagement than a flat, uniform surface. Your body must also work harder to regulate your internal temperature when exercising outdoors in hot or cold temperatures.
Burn more calories. The constantly changing outdoor environment creates more challenges and stress on the body. Wind resistance can make you burn more calories, especially when you’re running or cycling into a headwind. Walking or jogging on an uneven, changing terrain also requires more muscle engagement than a flat, uniform surface. Your body must also work harder to regulate your internal temperature when exercising outdoors in hot or cold temperatures.
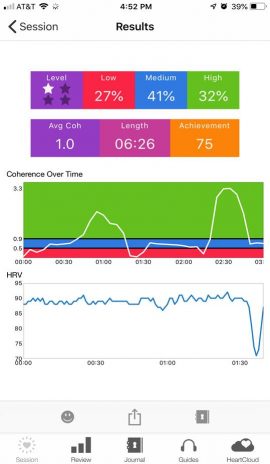 cer. One of her goals is to get stronger to be able to tolerate a chemotherapy treatment regimen. The team’s new COTA, Jay, decided to try HRV training to reduce pain and increase function. During the first session, the patient was able to briefly get into what is called neurological coherence, as indicated on the biofeedback device as the green zone. However, the pain quickly brought her out of coherence. Jay decided to try another technique. He asked her about one of her favorite places to be, and she told him it was Hawaii. Jay pulled up some Hawaiian music and talked her through the coherence steps, and she was very soon able to sustain coherence. What is really amazing is that she had been refusing physical therapy treatments due to pain, but after her session with Jay, she was able to participate in a full PT treatment, with a smile on her face. The biofeedback readings below show the spike in coherence when her favorite music and memories were introduced.
cer. One of her goals is to get stronger to be able to tolerate a chemotherapy treatment regimen. The team’s new COTA, Jay, decided to try HRV training to reduce pain and increase function. During the first session, the patient was able to briefly get into what is called neurological coherence, as indicated on the biofeedback device as the green zone. However, the pain quickly brought her out of coherence. Jay decided to try another technique. He asked her about one of her favorite places to be, and she told him it was Hawaii. Jay pulled up some Hawaiian music and talked her through the coherence steps, and she was very soon able to sustain coherence. What is really amazing is that she had been refusing physical therapy treatments due to pain, but after her session with Jay, she was able to participate in a full PT treatment, with a smile on her face. The biofeedback readings below show the spike in coherence when her favorite music and memories were introduced.
 It’s easy to get caught up in the day-to-day routine in this line of work. You have new programs you want to start, financial markers you strive to hit, and all of this trickles down to your team. However, every so often, you are reminded of why you chose this profession. It’s the people, their stories, their lives, and all they share.
It’s easy to get caught up in the day-to-day routine in this line of work. You have new programs you want to start, financial markers you strive to hit, and all of this trickles down to your team. However, every so often, you are reminded of why you chose this profession. It’s the people, their stories, their lives, and all they share.
 Kiran’s favorite recreation is playing with her two small children in her favorite place — her home. “I am a homebody and not very fond of traveling and adventuring. I love to stay home and spend quality time with my family and kids — this is the most beautiful place for me,” Kiran says.
Kiran’s favorite recreation is playing with her two small children in her favorite place — her home. “I am a homebody and not very fond of traveling and adventuring. I love to stay home and spend quality time with my family and kids — this is the most beautiful place for me,” Kiran says.
 Gordon Murray, Rehab Tech, has worked at North Mountain Medical and Rehab Center for over 14 years. Gordon has built many friendships with residents over the years due to his calm, gentle approach with residents. Gordon has a gift for motivating therapy patients, builds special bonds with them and has been referred to as “The Patient Whisperer” by his peers!
Gordon Murray, Rehab Tech, has worked at North Mountain Medical and Rehab Center for over 14 years. Gordon has built many friendships with residents over the years due to his calm, gentle approach with residents. Gordon has a gift for motivating therapy patients, builds special bonds with them and has been referred to as “The Patient Whisperer” by his peers!
 Miriam Janove, PT, is an August 2019 graduate of the University of Puget Sound, Washington.
Miriam Janove, PT, is an August 2019 graduate of the University of Puget Sound, Washington.
